Post-Acute Withdrawal Syndrome (PAWS)

When you stop using a substance regularly, you will encounter two distinct stages of withdrawal: an acute phase and a post-acute phase. The acute phase involves withdrawal symptoms related to your body’s attempt to detox and normalize after usual circulating levels of a substance decline. The post-acute phase, however, can linger for weeks, months, or even years after the initial withdrawal.
PAWS affects up to 90% of recovering opioid users and 75% of recovering alcohol and psychotropic misusers.1
Withdrawal is a normal part of the recovery process. Knowing what to expect during the withdrawal stage can help you better prepare. Assembling a trusted treatment team in advance can help you minimize withdrawal symptoms and improve your recovery experience.
What is PAWS?
Post-Acute-Withdrawal Syndrome (PAWS) involves a constellation of symptoms that often emerge weeks or months after you stop using a substance. PAWS is also known as post-withdrawal syndrome, prolonged withdrawal syndrome, and protracted withdrawal syndrome.
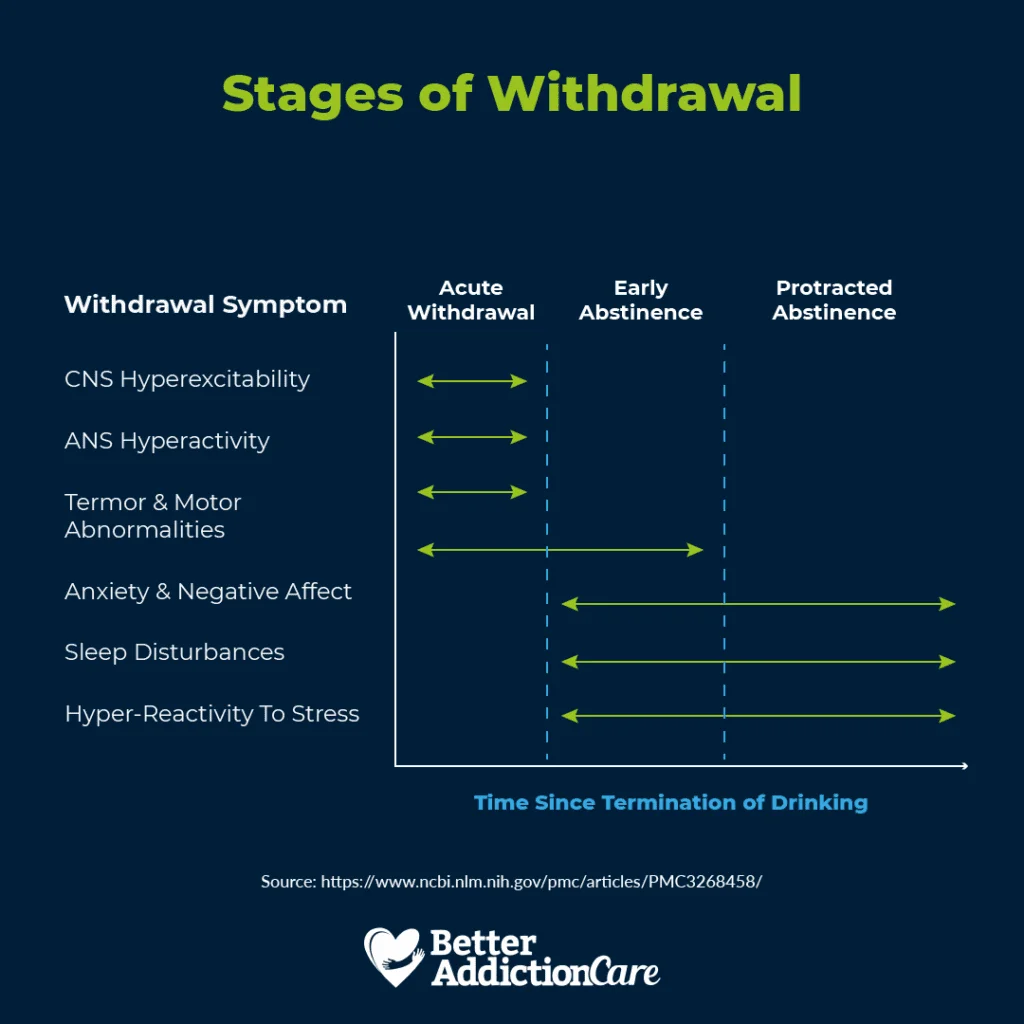
Acute symptoms of withdrawal are triggered by the nervous system’s response to the absence.2 In this early phase of withdrawal, you may experience tremors, hyperactivity, and hyperexcitability. Seizures generally occur within the first 24 to 48 hours of withdrawal.
After the initial acute withdrawal phase, sometimes called “early abstinence,” most patients experience fewer physical symptoms but continue to struggle with mild sleep disturbances, mood changes, and anxiety.
These post-acute withdrawal symptoms are often unpredictable, disappearing and reemerging without warning. Symptoms may or may not be related to a trigger, which can be unsettling for people who are just beginning their recovery process.
In some cases, the severity of the flare-up may be enough to trigger a relapse. For this reason, it’s essential to have ongoing support from a treatment support team.
Substances that are typically associated with PAWS include:2,3,4
- Alcohol: While acute alcohol withdrawal symptoms typically manifest within 48 to 72 hours after last alcohol consumption, lingering symptoms can surface three months after the acute phase has passed.
- Benzodiazepines: Benzodiazepines are commonly prescribed to treat anxiety and panic disorders, but due to their addictive nature, doctors usually only prescribe them for short-term use. Withdrawal can be particularly concerning in older adults who experience PAWS-related symptoms, such as confusion, ataxia, syncope, risk of falls, and fractures.
- Antidepressants: Research suggests that PAWS affects 30–50% of patients who stop antidepressant treatments. Acute withdrawal symptoms are common after discontinuation of psychotropics, and PAWS symptoms can linger for months to years after the last dose. Long-term use of antidepressants can lead to changes in serotonin pathways and brain function.
- Marijuana: Marijuana is known for its calming and relaxation properties. When a person stops using the substance, symptoms of depression and paranoia can linger and transition into PAWS. People who stop using marijuana may experience shifts in mood, sleep, appetite, and responses to stress.
- Opioids: Street drugs like heroin can lead to PAWS if not properly tapered during the withdrawal process. Medical supervision can make the withdrawal process safer and more effective.
- Stimulants: Similar to opioids, withdrawal from stimulants like cocaine and amphetamines should be discontinued in a controlled manner to minimize withdrawal symptoms. PAWS symptoms in people who previously used stimulants can include difficulty concentrating, anxiety, and depression.
Protracted Withdrawal Symptoms
In the final phase of abstinence, called “protracted abstinence,” patients may continue to experience symptoms. Some people report feeling indifferent about events that were once pleasurable before withdrawal of a substance, a condition called anhedonia. Addictive substances typically produce powerful surges of dopamine in the brain. When the substance is withdrawn, the brain needs time to resume the natural production of dopamine.
Protracted symptoms vary from substance to substance in terms of type, intensity, and duration.
Protracted symptoms may include:1,3,5
- Mood swings
- Insomnia and changes in sleep patterns
- Anxiety or panic (without clear stimulus)
- Craving prior abused substances
- Impaired cognition (difficulties with learning, problem-solving, and memory)
- Irritability
- Depressed mood
- Heightened sensitivity to stress
- Obsessive-compulsive behaviors
- Difficulty maintaining positive social relationships
- Pessimism
- Apathy
- Stomach upset
- Hostility
- Mood instability
- Fatigue
- Pain
- Weakness
What Factors Affect PAWS?
Each person’s recovery experience is different, and no one will experience PAWS the same way.
Factors that may affect PAWS include:
- The type of substance used
- How much and how frequently the substance was used
- How long the substance was used before withdrawal
- Other substances that were used
- Related co-occurring conditions
- Genetics
- Health status before withdrawal
Causes of Post-Acute Withdrawal Syndrome
There is no single cause for PAWS. Physical, emotional, and psychological factors influence this complex condition.
When you stop using a substance, your brain needs time to return to normal functioning. That process can take longer for some people than for others.
While the exact cause of PAWS remains unclear, experts suspect that changes in brain structure and function may play a role in symptoms.1 Some believe the condition is directly related to changes in neurotransmitter function resulting from prolonged substance misuse.
PAWS can occur after withdrawal from alcohol, benzodiazepines, opioids, and other psychoactive substances, but it occurs most frequently in those who misuse benzodiazepines.1
Evidence shows that the mesolimbic dopamine pathway is responsible for the positive reinforcing properties of substances like alcohol.2 Mesolimbic dopamine serves as a motivational learning signal. From this perspective, alcoholism is a learned addiction that has many rewards.
Is PAWS a Risk Factor for Relapse?
Yes, PAWS can be a risk factor for relapse, especially when symptoms persist or occur randomly during the early stages of recovery. Unless you have healthy coping strategies and a strong support network in place, you may be at a higher risk for relapse.
The compound effect of stressors and triggers can incrementally increase a person’s risk for relapse.
To prevent relapse, ongoing support is vital. This is why maintaining a supportive recovery network is essential for successful healing in the long term.
If you do relapse, you’re not alone. It’s a normal and natural part of the recovery process. Relapsing doesn’t mean you’ve failed. It may just be an indication that you need additional support. To get back on track, call our confidential helpline at 1-800-429-7690 to find a rehab near you.
Treatment for PAWS
Treatment options for PAWS vary and depend on the substance involved and the symptoms you’re experiencing. Your treatment provider may recommend medications, therapy, or a combination of the two to help you cope with PAWS symptoms. Since many post-acute withdrawal symptoms are emotional or psychological in nature, ongoing psychotherapy and counseling may be beneficial.
Therapists can support you throughout your recovery process by:
- Encouraging regular physical activity, nourishing food, and restful sleep
- Teaching impulse control and emotional regulation strategies
- Helping to identify and avoid triggers
- Build a positive support network
- Encouraging attendance at support groups like SMART Recovery, AA, or NA
- Suggesting self-care strategies to manage anxiety
- Teaching relaxation techniques
- Monitor for potential new or pre-existing co-occurring conditions
- Refer to other medical professionals as needed
- Finding healthy ways to manage stress or emotional distress

Medications may also help alleviate post-acute withdrawal symptoms. These include:5,6
- Naltrexone: This medication is often prescribed to treat alcohol and opioid addictions. Naltrexone blocks the effects of opioid receptors and decreases drug cravings.
- Antidepressants: Because of the high incidence of depression associated with substance withdrawal, antidepressants may help treat anxiety and mood changes that surface after a substance is discontinued.
- Acamprosate: This drug is commonly used to reduce withdrawal symptoms in people recovering from alcohol addiction, and it has been shown to be effective for some patients with PAWS. Acamprosate acts on neurotransmitters in the brain to reduce drug cravings.1
- Amantadine: Amantadine can significantly decrease fatigue in patients recovering from methamphetamine misuse.
If you are looking to quit drugs or alcohol, call our confidential 24/7 helpline and speak with a compassionate advisor who can connect you with a treatment program that best fits your needs. Begin your recovery journey today by contacting us at 1-800-429-7690.
Frequently Asked Questions About Post-Acute Withdrawal Syndrome
How Long Does it Take to Recover from Post-Acute Withdrawal Syndrome?
Full recovery from PAWS usually takes between 6 to 24 months, but each individual’s recovery path is different.7
Can You Prevent Post-Acute Withdrawal Symptoms?
While there is no way to completely avoid PAWS symptoms, learning how to manage and minimize them can dramatically improve your recovery experience and prevent relapses.
What Does PAWS Stand For?
PAWS is an abbreviation for post-acute withdrawal syndrome.
Does Everyone Experience Protracted Withdrawal?
Not necessarily. Symptoms of withdrawal are highly individualized and depend on many factors. It is impossible to predict with 100% accuracy who will experience protracted withdrawal.


