Drug Rehabs Covered by Health Insurance
Drug rehabs covered by health insurance offer a variety of treatment options, including inpatient and outpatient services, detox, counseling, and medication-assisted treatment. Health insurance covers drug and alcohol rehab services, and the Affordable Care Act mandates this coverage. The specifics of the services available vary by plan.

You should verify your benefits with your insurer to understand what is covered, as this helps minimize your out-of-pocket costs. Major insurance providers typically cover addiction treatment. To verify coverage, you need to gather your policy details and contact your insurer or a specialist.
According to Li, M.’s 2023 study, ‘Medical Costs of Substance Use Disorders in the US Employer-Sponsored Insurance Population’, substance use disorders (SUDs) cost the employer-sponsored insurance population approximately $35.3 billion annually, with alcohol-related disorders ($10.2 billion) and opioid-related disorders ($7.3 billion) being the most costly.
Does Insurance Cover Drug Rehab?
Yes. Under the Affordable Care Act (ACA), health insurance plans are required to cover drug and alcohol rehab services, including inpatient/outpatient treatment, detox, counseling, and medication. Coverage specifics, such as copays or network restrictions, vary by plan type (e.g., Medicaid, private, or marketplace plans). While most policies provide partial or full coverage, prior authorization or medical necessity documentation is required. Always verify benefits with your insurer to confirm eligibility and minimize out-of-pocket costs.
What Are the Drug Rehab Programs Covered by Health Insurance?
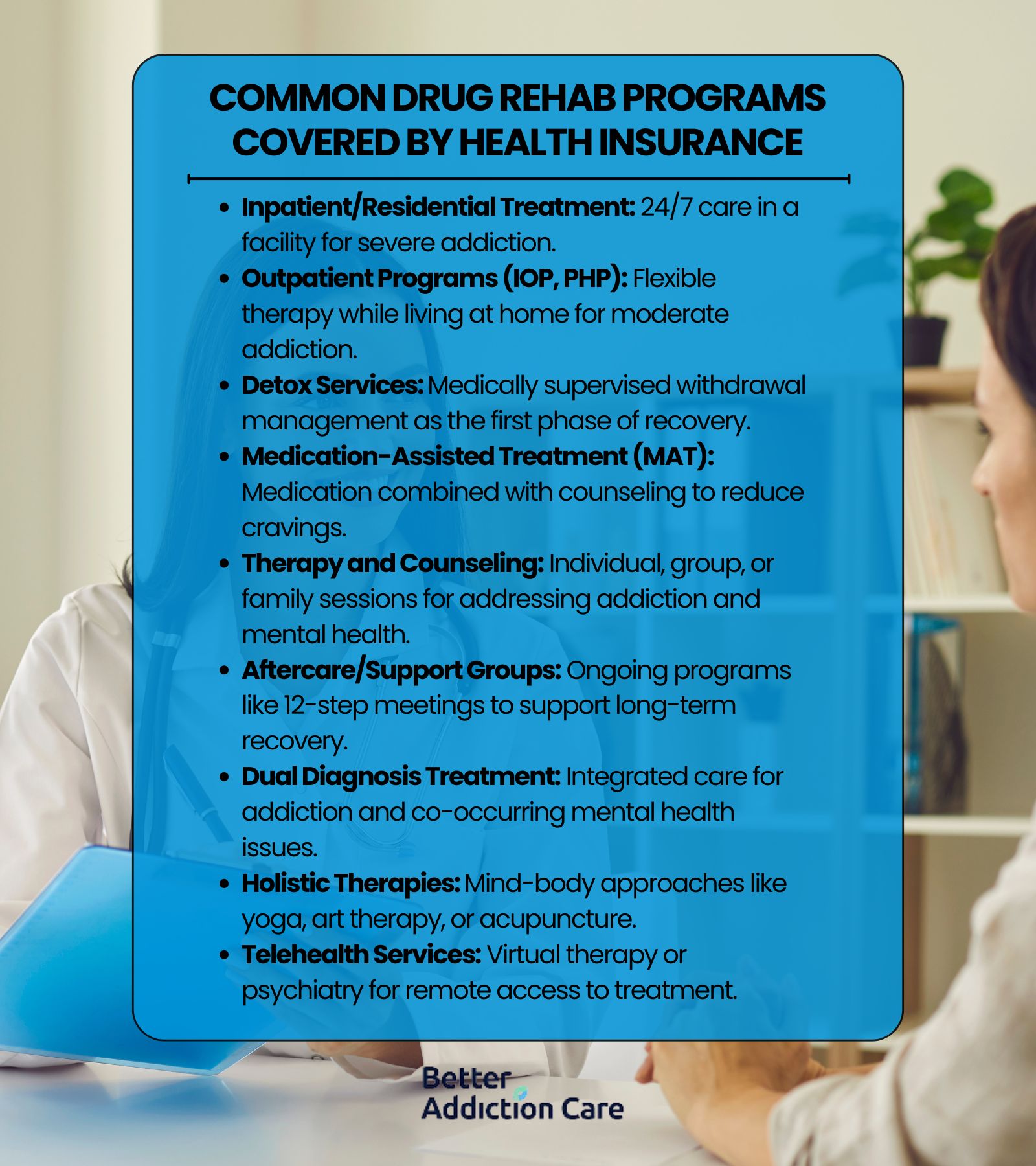
The drug rehab programs covered by health insurance include inpatient residential facilities, structured outpatient programs, medical detoxification services, and medication-assisted treatment options to support your recovery journey. Your insurance plan covers essential therapies like individual counseling, group sessions where you connect with peers, family therapy, and specialized treatment for co-occurring mental health conditions.
However, there is a concerning gap in awareness and utilization. According to Mojtabai, R.’s 2020 study, ‘Private health insurance coverage of drug use disorder treatment: 2005–2018’, 37.6% of people with drug use disorders don't know if their insurance covers treatment, and even among those with confirmed coverage, only 13.4% receive treatment services.
Here are the common drug rehab programs covered by health insurance:
-
Inpatient/Residential Treatment: Inpatient/Residential treatment is a structured program where you reside in a facility for 24/7 medical care and therapy. Health insurance covers this for severe addiction requiring intensive support.
-
Outpatient Programs (IOP, PHP): Outpatient programs (IOP, PHP) provide flexible treatment allowing you to live at home while attending therapy sessions. Insurance covers these for moderate needs or step-down care.
-
Detox Services: Detox services involve medically supervised withdrawal management to ensure safety. Insurance typically covers this as the critical first phase of recovery.
-
Medication-Assisted Treatment (MAT): Medication-Assisted Treatment (MAT) combines medications (e.g., buprenorphine, naltrexone) with counseling. Insurance covers MAT to reduce cravings and support long-term sobriety.
-
Therapy and Counseling: Therapy and counseling include individual, group, or family sessions to address trauma, triggers, and mental health. Insurance often covers these for comprehensive care.
-
Aftercare/Support Groups: Aftercare/support groups consist of ongoing programs like 12-step meetings or sober living homes. Many plans cover these to help you sustain recovery.
-
Dual Diagnosis Treatment: Dual diagnosis treatment offers integrated care for addiction and co-occurring mental health conditions (e.g., depression). Insurance covers this if you have overlapping diagnoses.
-
Holistic Therapies: Holistic therapies encompass mind-body approaches like yoga, art therapy, or acupuncture. Some plans cover these as complementary healing tools.
-
Telehealth Services: Telehealth services provide virtual therapy or psychiatry sessions for remote access. Insurers increasingly cover these for convenience and accessibility.
What Are the Major Insurance Providers and What They Cover?
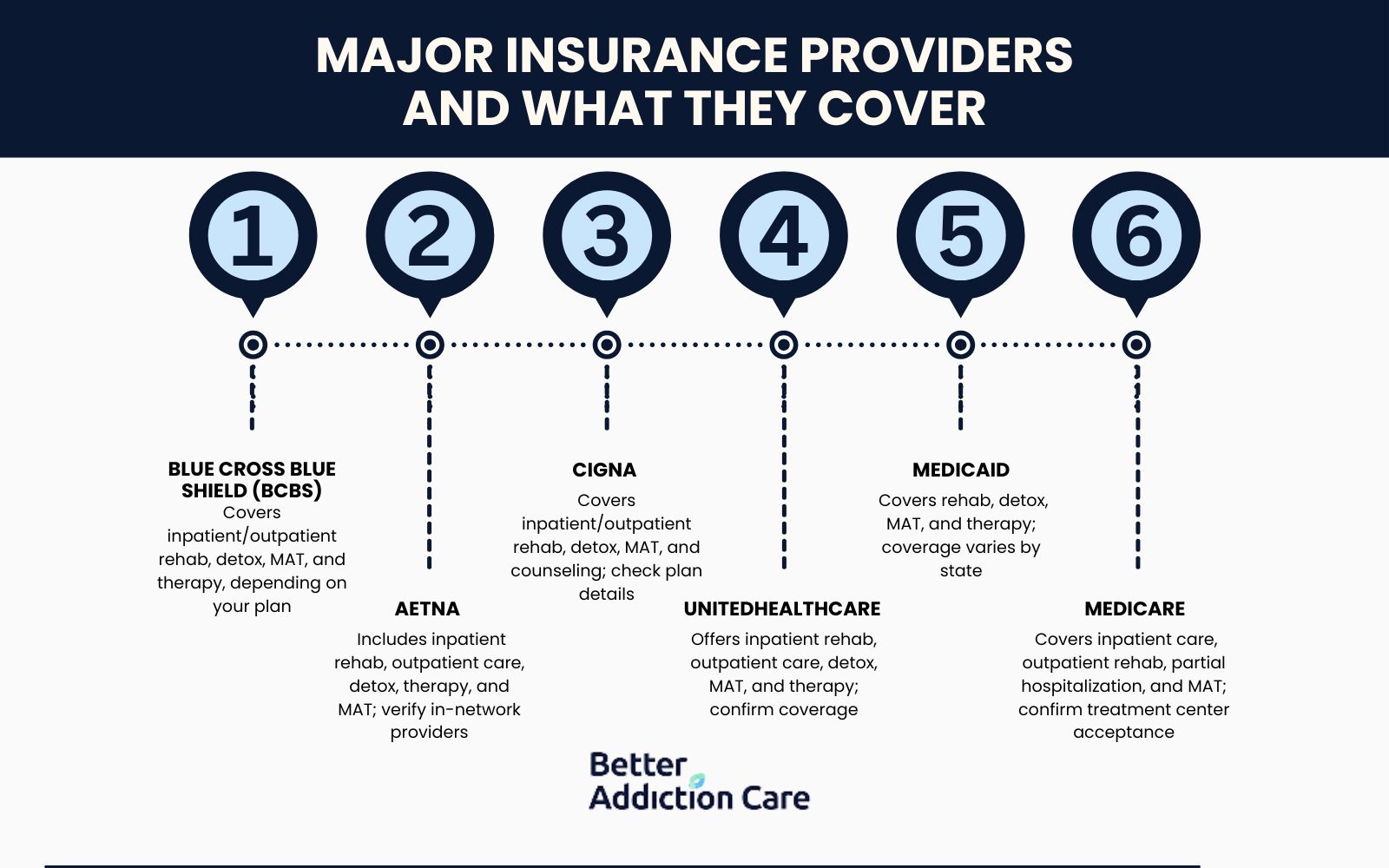
The major insurance providers covering addiction treatment include Blue Cross Blue Shield, Aetna, Cigna, UnitedHealthcare, Medicaid, and Medicare, offering coverage for rehab programs, detox services, and therapy. These insurers cover inpatient rehabilitation, outpatient care, medication-assisted treatment, and counseling sessions, though benefits vary by plan and location.
Here are the major insurance providers and what they cover:
Blue Cross Blue Shield (BCBS)
Blue Cross Blue Shield covers a wide range of addiction treatment services. With BCBS, you receive benefits for inpatient and outpatient rehab programs, detox services, medication-assisted treatment (MAT), and behavioral therapy. Coverage depends on your specific plan and state. Contact BCBS or your rehab provider directly to confirm which services are included in your benefits.
Aetna
Aetna includes drug and alcohol rehab in its health insurance plans. Your coverage includes inpatient rehab, outpatient programs, detox services, therapy sessions, and medication-assisted treatment. You need to verify in-network providers and confirm your treatment options with Aetna to ensure full access to covered services.
Cigna
Cigna provides addiction treatment coverage through a national network of rehab facilities. Your benefits include inpatient and outpatient rehab, medical detox, MAT, and individual or group counseling. Check your plan details or speak with Cigna or a participating treatment center to understand the services available to you.
UnitedHealthcare
UnitedHealthcare covers substance use treatment under its behavioral health services. Your insurance gives you access to inpatient rehab, outpatient care, detox programs, medication-assisted treatment, and therapy. Review your plan or call UnitedHealthcare to confirm coverage levels, deductibles, and participating facilities.
Medicaid
Medicaid covers essential addiction treatment services. You receive benefits for inpatient rehab, outpatient programs, detoxification, MAT, and therapy. Coverage varies by state, so you need to contact your state’s Medicaid office or a Medicaid-approved rehab center to find eligible services.
According to Olfson, M.’s 2018 study, ‘Impact Of Medicaid Expansion On Coverage And Treatment Of Low-Income Adults With Substance Use Disorders’, following the 2014 ACA Medicaid expansion, uninsurance rates among low-income adults with substance use disorders dropped from 34.4% to 20.4% in expansion states, highlighting Medicaid's critical role in addiction treatment coverage.
Medicare
Medicare includes substance use disorder treatment as part of its mental health coverage. You receive inpatient hospital care (Part A), outpatient rehab and therapy (Part B), partial hospitalization, and approved MAT prescriptions such as methadone and buprenorphine. To use your benefits, confirm that the treatment center accepts Medicare and that you meet any required criteria.
How to Verify Your Insurance Coverage?
To verify your insurance coverage for addiction treatment, gather your policy details and complete our verification form with your name, phone number, and email. Upon submission, you'll receive an assessment of your benefits, followed by a detailed explanation from a specialist about what your plan covers.
Most major providers cover addiction treatment services, including detox, rehabilitation, and medication-assisted treatment. Understanding these benefits eliminates financial uncertainty during your recovery journey.
We simplify this process at no cost to you. Our specialists quickly assess your coverage and explain your benefits clearly. To verify insurance, fill out our confidential form today. We'll connect you with treatment options tailored to your specific needs and coverage.
How to Choose the Right Drug and Alcohol Rehab Facilities?
To choose the right drug and alcohol rehab facilities, evaluate your specific needs first. Consider the severity of your addiction, whether you need inpatient or outpatient care, and which treatment approaches work best for you. Check accreditation, staff qualifications, and location factors. Financial considerations are essential—verify insurance coverage and payment options.
Our local drug and alcohol rehab facilities provide comprehensive assessments and personalized treatment plans with licensed professionals. We address both addiction and co-occurring mental health disorders while offering ongoing support and aftercare services for lasting recovery. Finding the right facility significantly improves your chances of successful sobriety.








