Accessing Rehab with Medicaid
Medicaid is a government-funded health insurance program that provides access to essential healthcare services, including addiction treatment, to low-income individuals and families, with coverage varying by state.

The role of Medicaid in rehab is to ensure access to comprehensive addiction treatment services, including detox, inpatient care, medications, and behavioral health support, by covering most or all costs for eligible low-income individuals and expanding access to care through initiatives like the Affordable Care Act.
According to Geissler, K. H.’s 2020 study, ‘Changes in Medicaid acceptance by substance abuse treatment facilities after implementation of federal parity’, 55.5% of substance use disorder (SUD) treatment facilities accepted Medicaid from 2002-2013. SUD treatment funding from Medicaid, Medicare, and private insurance increased from 43% to 49% between 2004-2014.
Medicaid covers a range of substance abuse treatment services, including detoxification, inpatient and outpatient rehabilitation, medications (e.g., Naloxone), counseling, behavioral therapies, case management, peer support, and opioid treatment programs (OTPs) in states with expanded Medicaid, ensuring comprehensive care for addiction recovery.
Challenges in accessing addiction treatment that accepts Medicaid include limited provider availability due to low reimbursement rates, geographic barriers in rural and underserved areas, a complex and time-consuming search process, financial and administrative burdens on providers, stigma and discrimination against Medicaid enrollees, lengthy waiting lists for treatment, variable coverage for addiction medications, and complexities in navigating eligibility and enrollment requirements.
What is Medicaid?
Medicaid is a joint federal and state program that helps cover medical costs for people with limited income and resources. It provides health insurance for adults and children with limited income. Medicaid covers approximately 83 million low-income people in the United States, making it the largest program providing medical and health-related services.
According to Shoulders, A.’s 2023 study, ‘Changes in Medicaid Fee-for-Service Benefit Design for Substance Use Disorder Treatment During the Opioid Crisis, 2014 to 2021’, every state Medicaid program now covers basic outpatient addiction treatment, a significant improvement from previous years. Almost all states (97%) have removed annual limits on addiction medications. However, gaps remain for more intensive services - 1 in 10 states doesn't cover intensive outpatient treatment, 1 in 8 states doesn't cover short-term residential care, and 1 in 3 states still doesn't cover long-term residential care. These findings come from a survey that included 46 states, with a detailed analysis of 38 states. While fewer states now require prior approvals and copayments for addiction services than before, these barriers to treatment remain common.
What Is The Role of Medicaid in Rehab?
The role of Medicaid in rehab is to provide coverage for drug and alcohol treatment services at approved facilities, covering most or all costs for eligible individuals. As a government health insurance program designed for low-income adults and children, Medicaid includes addiction treatment as part of its essential health benefits, particularly through expansions under the Affordable Care Act.
This coverage encompasses detox, inpatient care, medications, and ongoing behavioral health services, ensuring comprehensive care for substance use disorders (SUDs). By funding clinical treatments and recovery support, Medicaid helps reduce financial barriers to accessing care, enabling more individuals to pursue long-term recovery.
Additionally, Medicaid expansion has significantly improved access to behavioral health services, addressing gaps in treatment availability and supporting a more robust system of care for those in need.
According to Wodchis, W. P.’s 2007 study, ‘Effect of Medicaid Payment on Rehabilitation Care for Nursing Home Residents’, Medicaid Programs account for over 70% of government nursing home expenditures. Medicaid spending on nursing home care rose from $24.1 billion in 1990 to $38.9 billion in 1999. Between 33% and 50% of nursing home residents enter facilities specifically for rehabilitation therapy. The research examined 119,658 nursing home residents across six states from 1992-1995. Among Medicaid residents, those under Retrospective Cost-Based (RCB) payment received the most rehabilitation therapy (47% received therapy, averaging 252 minutes weekly), while those under Prospective Facility-Specific (PFS) payment received the least (30% received therapy). The average Medicaid payment rate was lowest under PFS and highest under Prospective Case-Mix (PCM) payment systems, which directly influenced rehabilitation service delivery.
What Does Medicaid Cover in Substance Abuse Treatment?
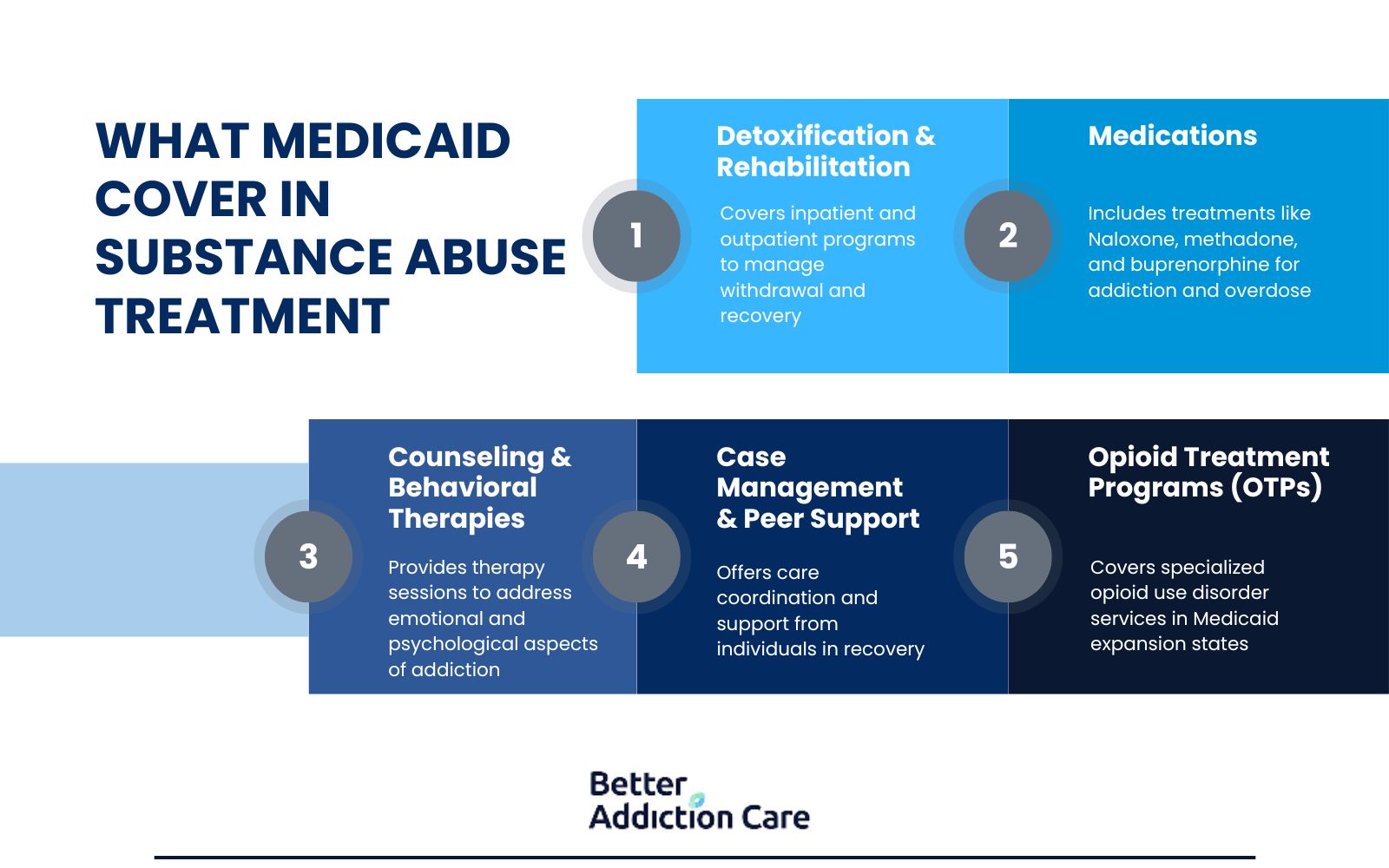
Medicaid covers detoxification, inpatient and outpatient rehabilitation, medications (e.g., Naloxone), counseling, behavioral therapies, case management, and peer support in substance abuse treatment.
-
Detoxification and Rehabilitation Services: Covered to manage withdrawal and provide structured care, including inpatient and outpatient programs.
-
Medications: Includes medications like Naloxone (for opioid overdose reversal) and those prescribed for addiction treatment (e.g., methadone, buprenorphine).
-
Counseling and Behavioral Therapies: Address psychological aspects of addiction through individual, group, or family sessions and support long-term recovery.
-
Case Management and Peer Support: Help coordinate care and provide guidance from individuals with lived experience in recovery.
-
Opioid Treatment Programs (OTPs): Covered in states that expanded Medicaid, along with other specialized services for opioid use disorder (OUD).
What Are The Challenges when Looking for Addiction Treatment that Takes Medicaid?

The challenges of Medicaid for addiction treatment include limited provider networks, geographic barriers to access, complex verification processes, and financial hurdles for facilities. Many individuals face long waiting lists, encounter stigma, struggle with medication coverage restrictions, and must navigate complicated eligibility requirements.
Here are the challenges of addiction treatment that take Medicaid:
-
Limited Provider Acceptance: A primary barrier is the scarcity of rehab facilities accepting Medicaid, especially in states with stricter eligibility criteria. Many providers opt out due to low Medicaid reimbursement rates, which often fail to cover operational costs, creating disparities in access for low-income individuals.
-
Geographic and Logistical Barriers: Rural and underserved areas face severe shortages of Medicaid-accepting providers, forcing patients to travel long distances for care. Transportation hurdles and sparse local options delay treatment initiation, exacerbating risks for those in crisis.
-
Complex Search and Verification Process: Finding Medicaid-eligible treatment requires persistent outreach: patients must individually contact facilities to confirm acceptance, navigate state-specific coverage rules, and coordinate with Medicaid offices. This process is time-consuming and discouraging for those already in vulnerable states.
-
Financial and Administrative Hurdles: Providers cite inadequate Medicaid reimbursements and burdensome billing processes as deterrents to participation. Facilities accepting Medicaid often face financial losses, leading to reduced service availability or refusal to treat Medicaid patients altogether.
-
Stigma and Discrimination: Despite broader shifts in public perception, Medicaid enrollees often encounter bias in treatment settings. Stereotypes about Medicaid recipients result in subpar care or reluctance from providers to offer equitable services.
-
Treatment Delays and Waiting Lists: Even when Medicaid-accepting facilities are identified, lengthy wait times—sometimes months—prevent timely access. Such delays endanger individuals needing urgent care, increasing the likelihood of relapse or overdose during the interim.
-
Variable Medication Coverage: Medicaid coverage for evidence-based addiction medications (e.g., buprenorphine) varies by state. Some providers avoid prescribing these treatments due to prior authorization requirements or reimbursement uncertainties, limiting access to gold-standard care.
-
Eligibility and Enrollment Complexities: Navigating Medicaid’s eligibility criteria, documentation demands, and enrollment steps overwhelms applicants, delaying their entry into treatment. Confusion about covered services further complicates the path to recovery.
What Should You Ask Before Using Medicaid for Addiction Treatment?
Questions you should ask before using Medicaid for addiction treatment include verifying your state's specific coverage for services like detox and counseling, checking for provider network restrictions, understanding prior authorization requirements, clarifying coordination with other insurance plans, and knowing your appeal rights if services are denied. Reviewing potential out-of-pocket costs, emergency care coverage, and available support services will also help you maximize your benefits.
Here is a list of questions that you should ask before using Medicaid for addiction treatment:
-
What specific addiction treatment services does Medicaid cover in my state?
Coverage varies by state, so confirm which services (e.g., detox, inpatient rehab, medications, counseling) are included and whether they align with your needs. -
Are there restrictions on treatment providers or facilities?
Verify if Medicaid requires you to use in-network providers or pre-approved facilities, and ask for a list of participating rehab centers in your area. -
Does Medicaid require prior authorization for certain treatments?
Some services (e.g., medication-assisted treatment) need pre-approval. Clarify the process and timeline to avoid delays in care. -
How does Medicaid coordinate with other insurance (if applicable)?
If you have additional insurance, understand which plan is primary and how benefits will be applied to avoid coverage gaps. -
What are my rights if coverage is denied?
Learn the appeals process for denied claims, including deadlines and documentation requirements, to challenge decisions effectively. -
Are there out-of-pocket costs for Medicaid-covered services?
Confirm copayments, deductibles, or other fees to budget accordingly, even with Medicaid coverage. -
Does Medicaid cover emergency or urgent addiction care?
Understand how crises (e.g., overdose, severe withdrawal) are handled and whether emergency services are fully covered. -
What support services (e.g., case management, peer counseling) are available?
Explore Medicaid-covered resources beyond medical care, such as transportation assistance or recovery coaching, to enhance your treatment plan.
Does Medicaid Cover Alternative Therapies?
Yes, Medicaid does cover alternative therapies, though coverage varies by state.
According to Steyer, T. E.’s 2002 study, ‘Medicaid reimbursement for alternative therapies’, 36 out of 46 state Medicaid programs (78.3%) provide coverage for at least one alternative therapy. The most commonly reimbursed therapies are chiropractic care (covered by 71.7% of programs), followed by biofeedback (21.7%), acupuncture (15.2%), and both hypnotherapy and naturopathy (10.8% each).
Does Medicaid Cover Sober Living Homes?
Medicaid does not cover sober living homes. Sober living homes are not considered a continuum of care and are usually not funded by state or government programs. Medicaid covers some costs of treatment at a rehabilitation facility, but the extent of coverage for sober living homes depends on the specific Medicaid plan.
What Are Some Alternative Insurance Options To Medicaid For Addiction Treatment?
Alternative insurance options to Medicaid for addiction treatment include private insurance plans (such as Aetna, Cigna, Blue Cross Blue Shield, and United Healthcare), Medicare for individuals 65 and older, TRICARE for military personnel and their families, Veterans Affairs healthcare for eligible veterans, Children's Health Insurance Program (CHIP) for families who don't qualify for Medicaid, coverage through the Affordable Care Act marketplace plans, Employee Assistance Programs (EAPs) offered by employers, and Indian Health Service coverage for Native Americans and Alaska Natives.
Private insurance plans come in several structures, including Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), Exclusive Provider Organizations (EPOs), Point of Service (POS) plans, and High Deductible Health Plans (HDHPs). Each offers different benefits regarding provider networks, referral requirements, and cost structures.
For seniors and some disabled individuals, Medicare provides coverage through various parts: Part A covers inpatient treatment, Part B covers outpatient services, Part D covers prescription medications for addiction treatment, and Medicare Advantage (Part C) combines these benefits.
The Affordable Care Act marketplace plans are particularly valuable for those who don't qualify for other programs, as they're required to cover substance use disorder treatment as an essential health benefit. Understanding the full scope of insurance for addiction treatment options helps individuals make informed decisions about their care and financial planning during recovery.
How to Find Local Rehab Facilities That Take Medicaid?
To find rehabilitation facilities that accept Medicaid, individuals should begin by researching Medicaid-certified facilities in their area through state Medicaid websites that provide provider directories. Working with Medicaid case managers is beneficial; these professionals navigate the complex healthcare system and identify appropriate treatment options.
Local health centers, nonprofit organizations, and faith-based groups provide valuable information about Medicaid-covered rehab services and referrals. Individuals seeking treatment must verify insurance coverage directly with facilities, as acceptance policies differ among centers.
At Better Addiction Care, we connect patients to treatment centers nationwide that accept Medicaid coverage, streamlining the process of finding suitable facilities. Better Addiction Care provides access to a database of local rehab facilities that accept Medicaid coverage.


