Hydroxyzine Interactions: Drugs, Alcohol & Safety Risks
Drug and alcohol interactions occur when multiple substances affect overlapping systems in the body. With hydroxyzine, the primary concern is stacked sedation, where more than one substance slows brain and nervous system activity simultaneously.

Key Takeaways:
- Hydroxyzine is not habit-forming, but it strongly depresses the central nervous system, which makes interactions with alcohol, sedatives, and certain medications potentially dangerous rather than benign
- The greatest risk comes from “stacked sedation,” where combining hydroxyzine with alcohol, opioids, benzodiazepines, sleep aids, or even some OTC products can impair breathing, coordination, judgment, and consciousness without immediate warning signs
- Many high-risk interactions involve everyday substances people underestimate, including cold and flu medicines, antihistamines, nighttime sleep aids, cannabis, and alcohol—especially in older adults or those taking multiple medications
- Safe use depends on awareness and communication, including avoiding alcohol, checking OTC labels, disclosing all substances to healthcare providers, and seeking medical guidance early—particularly for individuals in recovery or with underlying health conditions
Many people search for hydroxyzine interactions not out of curiosity, but out of concern—for their own safety or for someone they love.
Hydroxyzine is often prescribed to ease anxiety, help with sleep, or calm physical symptoms of distress. Because it’s sometimes viewed as a “safer” or non-addictive option, people may underestimate how risky certain combinations can be.
The reality is that mixing hydroxyzine with alcohol or other substances can quietly increase danger, especially in everyday situations like driving, managing anxiety, or navigating early recovery.
Understanding these interactions isn’t about fear—it’s about staying informed, preventing harm, and making choices that support long-term stability and healing.
What Is Hydroxyzine?
Hydroxyzine is a prescription medication commonly used to manage anxiety, tension, itching, nausea, and sleep difficulties.
In behavioral health settings, it’s often chosen because it does not belong to the benzodiazepine class and is not considered habit-forming in the traditional sense.
That said, hydroxyzine still has powerful calming effects on the brain and body.
It can slow reaction time, cause drowsiness, and affect mental clarity. These effects are part of why it works—but they’re also why interactions matter so much.
How Hydroxyzine Affects the Central Nervous System?
Hydroxyzine works by suppressing activity in the central nervous system (CNS).
It primarily blocks certain histamine receptors in the brain that are involved in alertness, wakefulness, and emotional arousal.
As a result, the brain receives fewer signals to stay stimulated, leading to sedation, relaxation, and a general slowing of nervous system activity.
Hydroxyzine tells the brain to ease off the accelerator. This can be helpful for calming anxiety, reducing agitation, or supporting sleep during periods of distress. However, the same mechanism that makes hydroxyzine effective also makes it vulnerable to interactions.
When other substances that slow the CNS are introduced, the nervous system may become over-suppressed, interfering with breathing, coordination, and awareness.
This is why interaction risks with hydroxyzine are less about the medication itself and more about what else is present in the body at the same time.
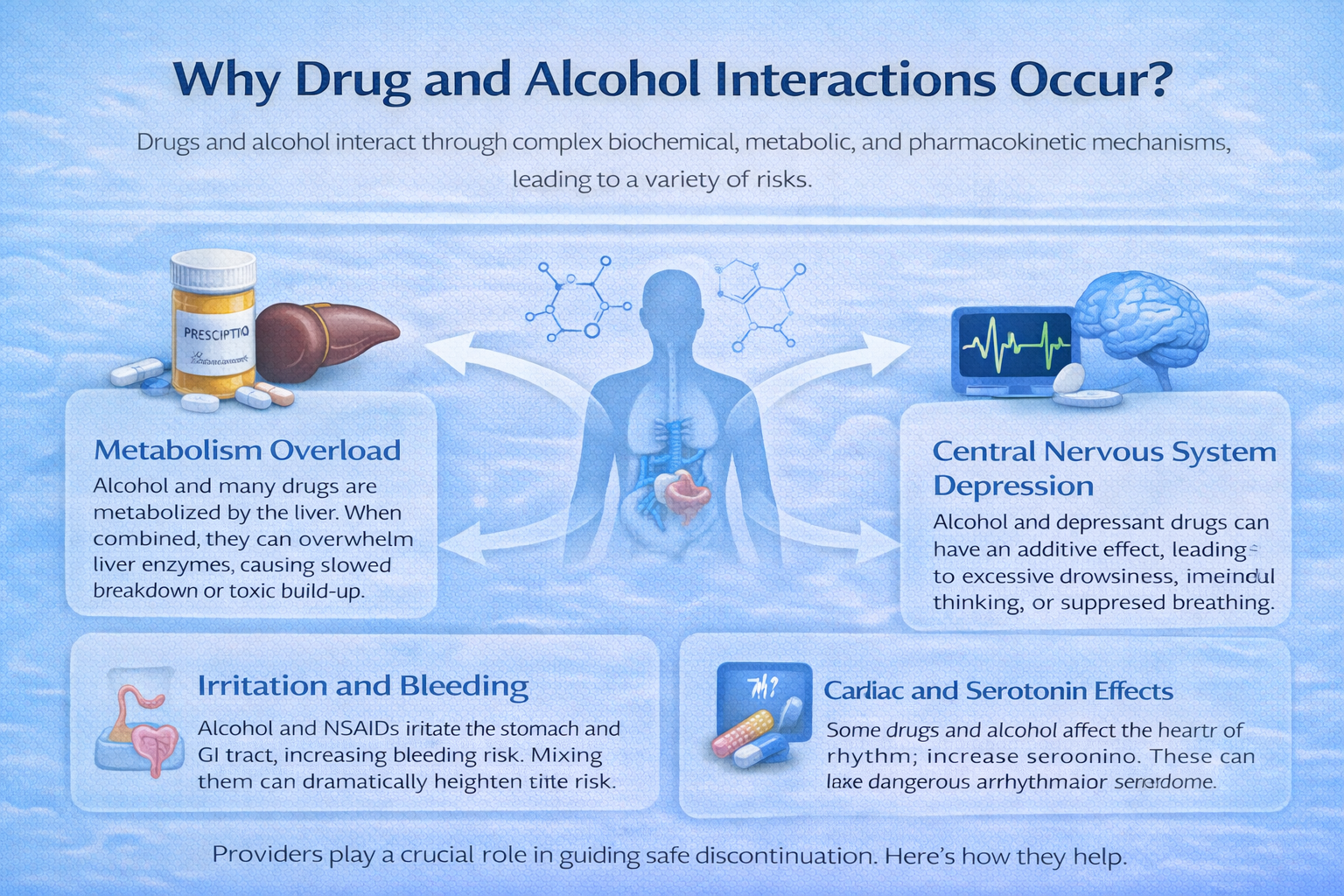
Why Drug and Alcohol Interactions Occur?
Drug and alcohol interactions occur when multiple substances affect overlapping systems in the body.
With hydroxyzine, the primary concern is stacked sedation, where more than one substance slows brain and nervous system activity simultaneously.
When substances are combined, they can:
-
Intensify drowsiness and mental fog beyond expected levels
-
Impair coordination, balance, and judgment
-
Suppress breathing, reflexes, and alertness
-
Increase the likelihood of falls, accidents, and unsafe decisions
What makes these interactions particularly dangerous is that they often don’t feel immediately alarming. Instead of sudden symptoms, people may feel progressively heavier, slower, or disconnected.
By the time warning signs appear, judgment may already be impaired, making it harder to recognize when help is needed.
Hydroxyzine and Alcohol Interactions
Alcohol is one of the most dangerous substances to mix with hydroxyzine because both act as central nervous system depressants. Together, they amplify each other’s effects rather than balancing out.
When combined, hydroxyzine and alcohol can cause:
-
Extreme drowsiness or sudden, uncontrollable sleep episodes
-
Confusion, disorientation, or memory gaps
-
Slowed reaction time and impaired decision-making
-
Increased risk of falls, vehicle accidents, or injuries
-
In difficult situations, slowed or shallow breathing
For individuals in recovery, alcohol adds an emotional and psychological layer of risk. Even small amounts can lower inhibitions, weaken coping skills, and increase impulsivity.
What begins as physical sedation can quickly turn into emotional vulnerability, making relapse or risky behavior more likely.
Prescription Drug Interactions With Hydroxyzine
Hydroxyzine can interact dangerously with several categories of prescription medications, particularly those that also affect the central nervous system.
These interactions may not be obvious at first, especially when medications are prescribed by different providers.
High-risk categories include:
-
Opioid pain medications, which can dangerously suppress breathing
-
Benzodiazepines and other sedatives leading to profound sedation and confusion
-
Sleep medications, which may cause unexpected loss of consciousness
-
Certain antidepressants or antipsychotics, which can amplify CNS and heart rhythm effects
Because symptoms may develop gradually, people may not realize a combination is unsafe until functioning is already impaired.
This is why medical oversight and full disclosure of all medications are critical when hydroxyzine is part of a treatment plan.
Over-the-Counter Medication Interactions
Many people assume over-the-counter medications are harmless simply because they don’t require a prescription.
Unfortunately, this assumption leads to some of the most common and overlooked interaction risks.
OTC products that may interact with hydroxyzine include:
-
Cold and flu remedies
-
Antihistamines
-
Nighttime sleep aids
-
Motion sickness medications
Hydroxyzine itself has antihistamine properties, so combining it with similar OTC products can lead to unexpected over-sedation, confusion, dry mouth, vision changes, or even heart rhythm disturbances.
Older adults are especially vulnerable, as their bodies process medications more slowly and are more sensitive to cumulative effects.
Hydroxyzine and Recreational or Non-Prescribed Substances
Mixing hydroxyzine with recreational or non-prescribed substances significantly increases risk, particularly outside of medical supervision. These combinations often introduce unpredictability rather than balance.
This includes:
-
Cannabis, which may increase confusion, anxiety, or panic, rather than calm
-
Illicit opioids, which dramatically raise the risk of respiratory suppression
-
Stimulants, which can mask sedation temporarily before causing sudden crashes
For individuals managing anxiety, trauma, or emotional dysregulation, these combinations can worsen mood instability, increase impulsive behavior, and interfere with recovery goals.
What feels like short-term relief may lead to longer-term destabilization.
Who Is at Higher Risk From Interactions?
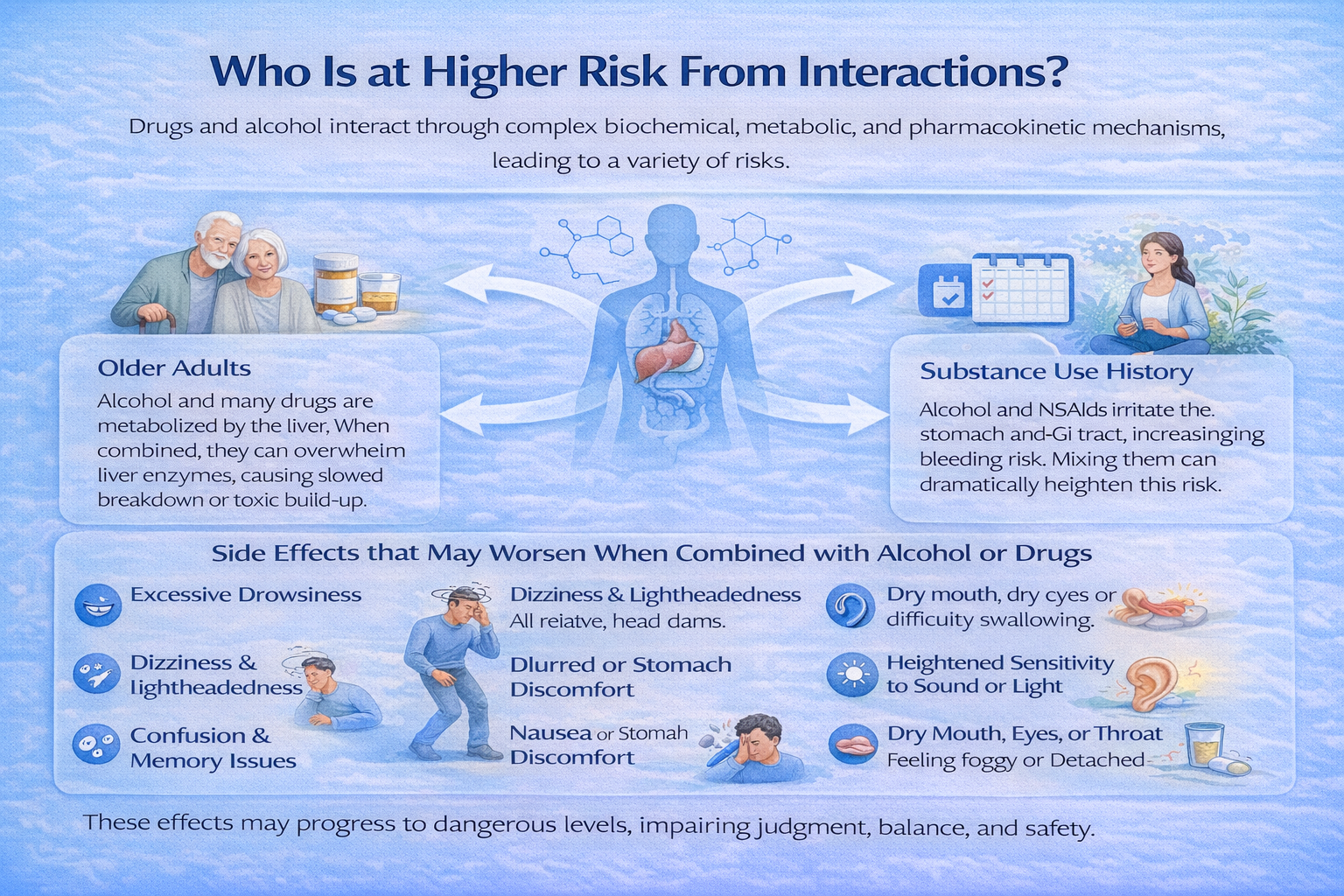
Certain populations are more sensitive to hydroxyzine interactions due to physiological, psychological, or situational factors.
Higher-risk groups include:
-
Older adults
-
People taking multiple medications
-
Individuals with breathing or heart conditions
-
Those with a history of substance use or dependency
-
People in early recovery or active relapse prevention
For these individuals, even moderate interactions can lead to outsized consequences, including injury, hospitalization, or setbacks in mental health stability.
Common Side Effects That May Worsen With Interactions
Hydroxyzine’s typical side effects may become significantly more intense when combined with other substances, particularly those that also affect the central nervous system.
These effects can appear suddenly or build over time, even at previously tolerated doses.
These may include:
-
Excessive drowsiness or persistent fatigue — Feeling unusually sleepy or lethargic throughout the day, even after adequate rest; may interfere with daily responsibilities and alertness.
-
Dizziness or lightheadedness, especially when standing or walking — A sense of unsteadiness or vertigo that increases the risk of falls or accidents, often worsening with sudden movements.
-
Blurred or double vision — Difficulty seeing clearly, objects appearing doubled, or temporary loss of focus, which can affect reading, driving, or other precision tasks.
-
Confusion, slowed thinking, or memory lapses — Struggling to process information, remember recent events, or make decisions; may feel mentally sluggish or foggy.
-
Difficulty focusing, problem-solving, or completing tasks — Reduced cognitive performance, trouble concentrating on work or school tasks, and challenges with planning or executing activities.
-
Slurred speech or delayed reaction time — Speech may become slow or unclear, and reflexes or responses to external stimuli may be noticeably delayed.
-
Poor coordination or unsteady gait — Difficulty maintaining balance, walking steadily, or performing fine motor tasks, increasing the risk of tripping or falling.
-
Headache or pressure-like sensations — Persistent or dull headaches, tightness around the head, or a feeling of internal pressure, which can worsen with stress or dehydration.
-
Nausea or stomach discomfort related to slowed digestion — Queasiness, bloating, or indigestion caused by decreased gastrointestinal motility.
-
Increased sensitivity to light or sound — Feeling easily overwhelmed by bright lights, loud noises, or crowded environments, which may exacerbate discomfort.
-
Dry mouth, dry eyes, or difficulty swallowing — Reduced saliva or tear production, making eating, speaking, or blinking uncomfortable.
-
A general feeling of mental “fog” or detachment from surroundings — Feeling disconnected, spaced out, or “out of it,” which can impair decision-making and awareness of one’s environment.
What may initially feel like mild discomfort can quickly become unsafe, especially during activities that require alertness, balance, or quick decision-making—such as driving, operating machinery, cooking, or caring for others.
Warning Signs of a Dangerous Interaction
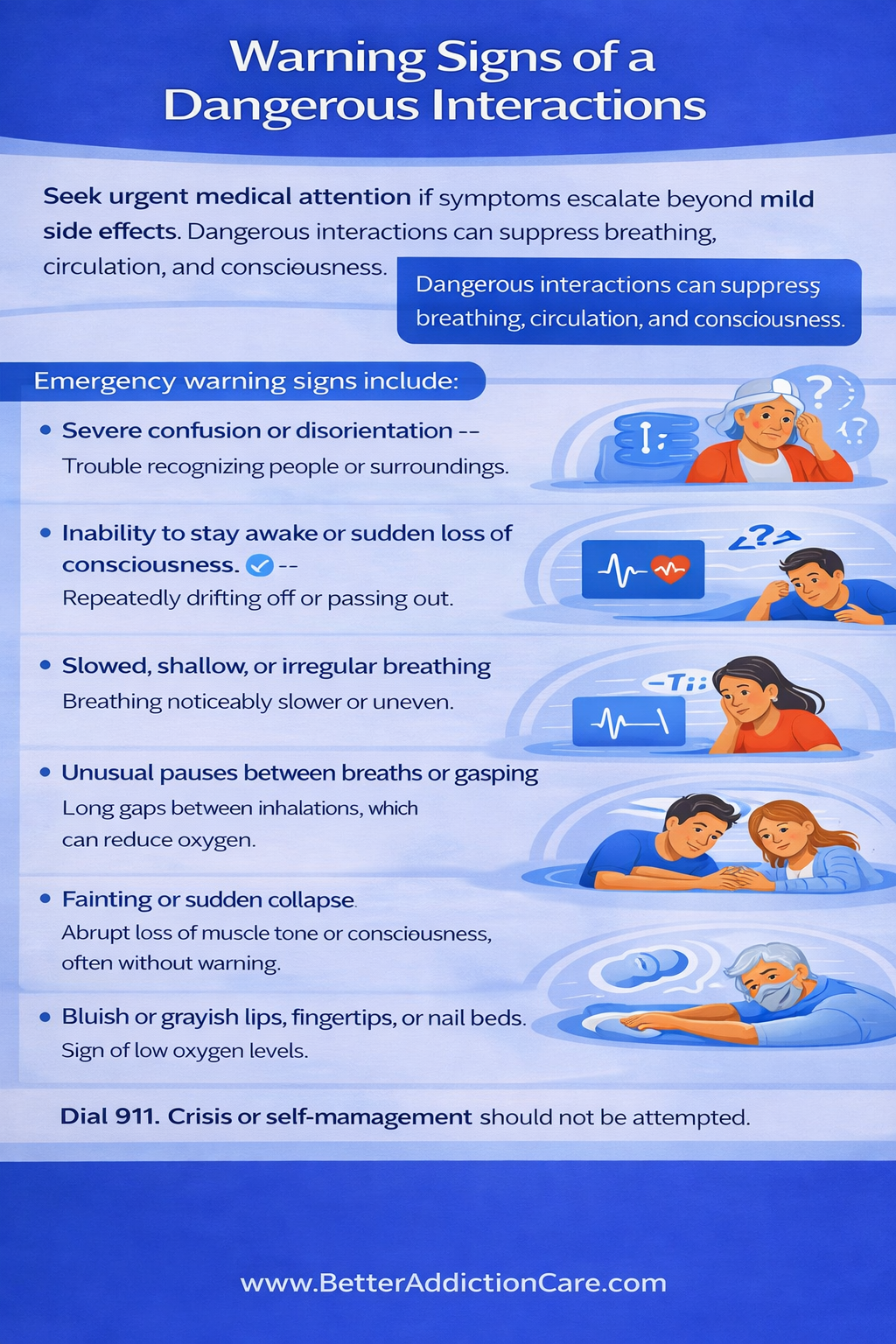
Seek urgent medical attention if symptoms escalate beyond mild or expected side effects.
Dangerous interactions can suppress the nervous system and interfere with breathing, circulation, and consciousness.
Emergency warning signs include:
-
Severe confusion or disorientation — Trouble recognizing people or surroundings, difficulty understanding simple instructions, or appearing mentally “lost,” which may signal significant central nervous system suppression.
-
Inability to stay awake or sudden loss of consciousness — Repeatedly drifting off, collapsing into sleep without warning, or becoming completely unconscious, even when stimulated.
-
Slowed, shallow, or irregular breathing — Breathing that is noticeably slower than normal, unusually quiet, uneven, or labored, indicating depressed respiratory function.
-
Unusual pauses between breaths or gasping — Long gaps between inhalations, gasping for air, or breathing that appears strained or interrupted, which can reduce oxygen delivery to the brain.
-
Fainting or sudden collapse — Abrupt loss of muscle tone or consciousness, often without warning, increasing the risk of serious injury from falls.
-
Bluish or grayish lips, fingertips, or nail beds — A visible sign of low oxygen levels in the blood, suggesting that the body is not getting enough oxygen to vital organs.
-
Weak, slow, or irregular pulse — A heartbeat that feels faint, abnormally slow, or uneven, potentially reflecting cardiovascular instability.
-
Extreme difficulty speaking or forming words — Slurred, garbled, or incoherent speech, or an inability to respond verbally at all, indicating impaired brain function.
-
Unresponsiveness to voice, touch, or pain — Failure to wake or react when spoken to, shaken, or gently stimulated, signaling a potentially life-threatening level of sedation.
-
Seizure-like activity or uncontrolled muscle movements — Shaking, jerking, stiffening, or twitching that is involuntary, which may indicate severe neurological distress.
These symptoms signal a medical emergency—not side effects to wait out, self-manage, or dismiss. Prompt intervention can be life-saving, especially when multiple substances are involved.
Safe Use and Risk-Reduction Guidelines
Reducing interaction risk involves awareness, communication, and self-protection.
General precautions include:
-
Avoiding alcohol while taking hydroxyzine
-
Reading OTC labels carefully and consistently
-
Sharing a full medication and substance history with healthcare providers
-
Never combining medications without guidance
-
Using extra caution during periods of stress, grief, or emotional instability
Risk reduction isn’t about perfection—it’s about protecting progress, safety, and stability.
Hydroxyzine and Dependency or Misuse Considerations
Hydroxyzine is not classified as an addictive medication, and it does not produce the cravings or compulsive drug-seeking behavior typically associated with substance use disorders.
However, misuse and psychological reliance can still occur, particularly when the medication is used as a primary way to escape emotional discomfort, force sleep, or blunt anxiety without addressing its underlying causes.
In recovery and mental health settings, this kind of over-reliance can be subtle.
Sedation may temporarily quiet racing thoughts or emotional distress, but when used repeatedly as a coping shortcut, it can quietly replace healthier strategies such as emotional regulation, therapy-based skill building, or processing stress with appropriate support.
Over time, individuals may come to feel they cannot relax, sleep, or function without the medication—even if no physical addiction is present.
Another concern is tolerance and escalating use. While hydroxyzine does not cause classic withdrawal, some people may feel compelled to increase frequency or dosage to achieve the same calming effect. This can raise the risk of side effects such as excessive drowsiness, cognitive dulling, dry mouth, or impaired coordination—especially in older adults or those taking other sedating medications.
Misuse risks are also higher when hydroxyzine is combined with other central nervous system depressants, including alcohol, opioids, or benzodiazepines.
These combinations can amplify sedation and impair breathing, judgment, and reaction time, increasing the risk of accidents or medical complications.
For these reasons, awareness, clear boundaries, and honest communication with healthcare providers are essential.
When used intentionally, monitored appropriately, and paired with non-medication coping strategies, hydroxyzine can be a helpful short-term aid. Without those safeguards, however, it may shift from a useful support into a hidden obstacle to long-term emotional resilience and recovery.
When to Speak With a Doctor or Specialist?
Professional guidance becomes especially important when hydroxyzine is part of a broader treatment picture.
Because interaction risks often build quietly over time, reaching out early can prevent complications before they escalate.
It’s essential to speak with a doctor, psychiatrist, or other qualified specialist if:
-
Multiple medications are involved, particularly those that affect mood, sleep, pain, or alertness, as overlapping effects may increase sedation or confusion.
-
Alcohol use is ongoing or was recently discontinued, since changes in drinking patterns can significantly alter how the body responds to medications.
-
There is a personal history of substance use disorder, even if recovery is well established, because vulnerability to misuse or unsafe combinations may still exist.
-
Anxiety, agitation, or sleep problems are worsening rather than improving, which may signal that the current approach isn’t addressing the root issue.
-
Side effects feel unmanageable or interfere with daily functioning, such as difficulty staying awake, thinking clearly, or staying emotionally balanced.
Reaching out for professional input is not a sign of weakness or failure.
It’s a protective and proactive step—one that supports safety, preserves progress, and helps ensure that treatment aligns with both physical health and long-term emotional recovery.
FAQs
Combining hydroxyzine with alcohol significantly increases sedation and safety risks and is generally discouraged. Both substances slow down the central nervous system, which can lead to extreme drowsiness, poor coordination, slowed thinking, and impaired judgment.
Hydroxyzine may be used in some recovery settings, particularly when anxiety, sleep disruption, or acute distress is present. However, safety depends on transparency, monitoring, and intention. While it is not considered addictive, it can still be misused for its calming effects or combined unsafely with other substances.
Yes. Many anxiety medications also affect the central nervous system. When combined with hydroxyzine, their sedating effects can intensify, leading to excessive drowsiness, slowed thinking, confusion, or difficulty concentrating. These effects may interfere with daily functioning and increase safety risks. Medical supervision is essential when multiple medications are involved, especially during periods of emotional stress or medication changes.
Waiting a certain amount of time does not reliably eliminate interaction risk. Hydroxyzine can remain active in the body longer than people expect, and combining substances—even hours apart—can still lead to overlapping effects. Because individual metabolism and sensitivity vary, timing alone is not a dependable safety strategy.
Yes. Hydroxyzine can impair reaction time, focus, and coordination on its own. When combined with alcohol, sleep aids, or other sedating substances, these effects can become more pronounced and unpredictable. This increases the risk of driving accidents, workplace injuries, and errors that could have serious consequences.
If you’ve already combined hydroxyzine with alcohol or another substance, pay close attention to how your body responds. Increasing drowsiness, confusion, slowed breathing, or difficulty staying awake are warning signs that require medical attention. If symptoms feel severe or escalate, seeking urgent care is the safest step. Reaching out for help is not an overreaction—it’s a protective response.