Percocet Addiction: Signs, Symptoms, Withdrawal, and Treatment
Percocet addiction is the reliance on a prescription pain medication, that is a combination of oxycodone and acetaminophen. Percocet is prescribed for moderate to severe pain relief and it poses a high addiction risk, particularly when used in larger doses or outside prescribed guidelines. Percocet addiction affects approximately 2.5 million individuals, making it one of the most common forms of prescription painkiller abuse according to “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health,” published in 2023 by the Substance Abuse and Mental Health Services Administration.

Percocet addiction is the reliance on a prescription pain medication, that is a combination of oxycodone and acetaminophen. Percocet is prescribed for moderate to severe pain relief and it poses a high addiction risk, particularly when used in larger doses or outside prescribed guidelines. Percocet addiction affects approximately 2.5 million individuals, making it one of the most common forms of prescription painkiller abuse according to “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health,” published in 2023 by the Substance Abuse and Mental Health Services Administration.
The signs of Percocet addiction are diverse, including increased secrecy about usage, frequent attempts to obtain refills, and visiting multiple doctors to secure additional prescriptions. Individuals often show an unusual preoccupation with maintaining a steady supply of the drug.
The symptoms of Percocet addiction include both physical and psychological changes. Persistent cravings drive individuals to prioritize obtaining and using Percocet over other responsibilities, while anxiety and mood swings create emotional instability. A notable increase in tolerance leads to progressively higher doses required to achieve the same level of pain relief or satisfaction, escalating the cycle of addiction. Many individuals also lose interest in hobbies, relationships, and social activities they once enjoyed, as the focus shifts entirely toward the need for the drug.
The withdrawal for Percocet addiction includes symptoms such as nausea, muscle pain, anxiety, insomnia, and excessive sweating. Withdrawal symptoms often peak within a few days after stopping Percocet and present both physical and emotional challenges. Withdrawal anxiety is a common symptom of Percocet withdrawal, typically lasting five to 14 days after stopping the medication, according to the 2019 study titled “Effective Management of Opioid Withdrawal Symptoms: A Gateway to Opioid Dependence Treatment” in The American Journal on Addictions.
The treatment for Percocet addiction involves a comprehensive approach with medical detox, counseling, and support groups. Medical supervision addresses withdrawal symptoms, while therapy uncovers the root causes of Percocet addiction, guiding individuals toward long-term recovery.
What is Percocet Addiction?
Percocet addiction is a type of substance use disorder that involves the compulsive use of Percocet despite harmful consequences. This addiction develops when an individual becomes dependent on Percocet, a combination of oxycodone and acetaminophen used for pain relief, leading to an overwhelming need to use the drug regularly. Those struggling with Percocet addiction exhibit behaviors driven by cravings, prioritize drug use over personal and professional responsibilities, and require increasingly higher doses to achieve the desired effects.
Percocet addiction is considered an opioid use disorder because the active ingredient is oxycodone. According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), approximately 0.37% of the adult population in the United States is affected by opioid use disorder, which includes Percocet addiction.
What is Percocet?
Percocet is a prescription medication that combines oxycodone, a potent semisynthetic opioid, with acetaminophen, a non-opioid pain reliever, to manage moderate to severe pain. Each tablet typically contains between 2.5 mg to 10 mg of oxycodone and 325 mg of acetaminophen, with variations in dosage depending on the prescription. This combination provides effective pain relief by targeting pain through two mechanisms: oxycodone's action on opioid receptors to block pain signals and acetaminophen's effect on reducing fever and minor aches.
Percocet information:
|
Strength |
Oxycodone |
Acetaminophen |
Usual Adult Dosage |
Maximum Daily Dose |
Route of Administration |
|
2.5 mg/325 mg |
2.5 mg |
325 mg |
1 to 2 tablets every 6 hours as needed |
12 tablets |
Oral |
|
5 mg/325 mg |
5 mg |
325 mg |
1 tablet every 6 hours as needed |
12 tablets |
Oral |
|
7.5 mg/325 mg |
7.5 mg |
325 mg |
1 tablet every 6 hours as needed |
8 tablets |
Oral |
|
10 mg/325 mg |
10 mg |
325 mg |
1 tablet every 6 hours as needed |
6 tablets |
Oral |
Percocet is prescribed as an oral tablet but is misused by crushing and snorting, injecting, chewing, or taking sublingually (under the tongue) to accelerate absorption and intensify effects. These methods bypass standard digestive processing, increasing the risk of overdose, dependence, and severe health complications.
What are the Signs, Symptoms and Side Effects of Percocet Addiction?
The signs, symptoms and side effects of Percocet are physical and psychological and include general side effects from taking Percocet as well as addiction symptoms, withdrawal symptoms and overdose symptoms.
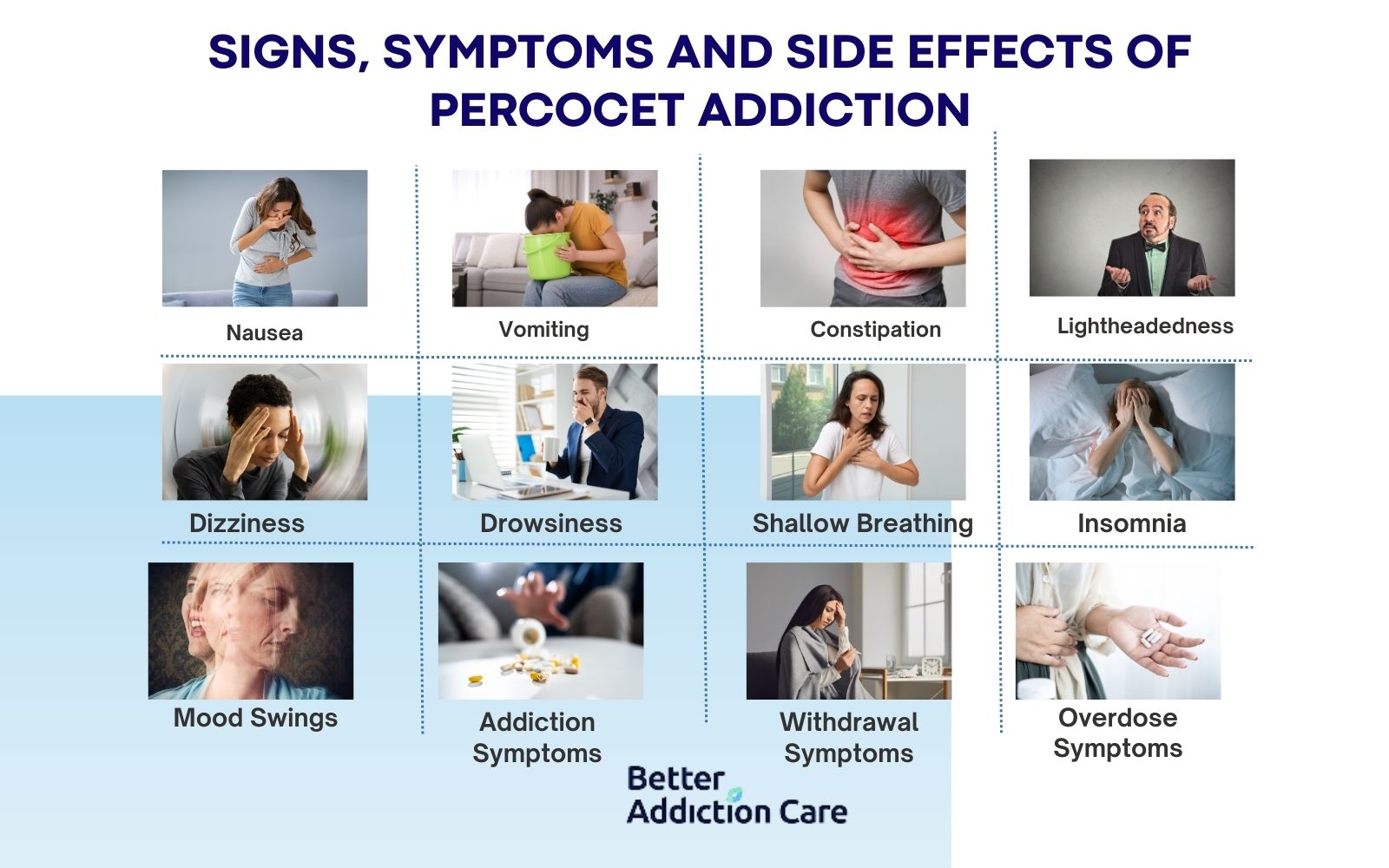
The signs, symptoms and side effects of Percocet addiction are listed below:
-
Nausea: Nausea is a physical side effect of Percocet, resulting from the drug’s impact on the digestive and central nervous systems. By slowing down gastrointestinal processes, Percocet commonly leads to nausea, especially during dosage changes or initial use.
-
Vomiting: Vomiting is a physical side effect and withdrawal symptom of Percocet. It often follows nausea and intensifies during withdrawal as the brain’s vomiting center responds to the absence of the drug, indicating the body’s dependence on Percocet.
-
Constipation: Constipation is a physical side effect of Percocet, caused by the drug’s effects on gut motility. Percocet binds to receptors in the intestines, slowing muscle contractions and leading to significant constipation, particularly with prolonged use. Opioid-induced constipation (OIC) affects 45-90% of patients taking opioids for pain management according to the National Comprehensive Cancer Network (NCCN).
-
Lightheadedness: Lightheadedness is a physical side effect of Percocet, occurring due to the drug’s depressant effects on the central nervous system. This effect impacts balance and reaction time, particularly at higher doses, as Percocet lowers blood pressure and oxygen flow.
-
Dizziness: Dizziness is a physical side effect of Percocet, linked to its sedative effects that slow brain activity and impair balance. This side effect is present during initial use or increased dosages, as the drug affects the neurological functions responsible for spatial awareness.
-
Drowsiness: Drowsiness is a physical side effect of Percocet, resulting from its central nervous system depressant properties, which slow bodily functions and induce sedation. While beneficial for pain relief, drowsiness frequently impacts daily activities and overall alertness.
-
Shallow Breathing: Shallow breathing is a physical side effect and symptom of Percocet use, especially at high doses. Oxycodone, the opioid in Percocet, slows respiratory function, leading to dangerously low oxygen levels in the body. This effect reduces oxygen flow to critical organs like the brain, potentially causing symptoms like dizziness, confusion, or, in severe cases, unconsciousness. Respiratory depression is a common and dangerous opioid side effect, particularly in cases of misuse or overdose.
-
Insomnia: Insomnia is a physical and psychological side effect of Percocet that disrupts sleep cycles, leading to difficulties in falling and staying asleep. A study out of 8,433 participants, 2,115 (25%) reported experiencing insomnia, while 4,200 (50.3%) indicated they used opioids. The findings showed a higher likelihood of insomnia among opioid users compared to non-users, even when accounting for other variables, according to Serdarevic et al. 2017, titled "The Association between Insomnia and Prescription Opioid Use: Results from a Community Sample in Northeast Florida," .
-
Mood Swings: Mood swings are a psychological symptom and side effect of Percocet addiction, characterized by sudden and intense changes in emotional states. The drug’s impact on brain chemistry creates fluctuations in mood, often producing a cycle of euphoria followed by irritability or anxiety. These mood shifts contribute to the psychological dependence on Percocet, as individuals may continue using it to experience temporary relief from negative emotions.
-
Addiction Symptoms: Addiction symptoms are psychological and behavioral signs of Percocet use, involving compulsive drug-seeking behaviors, neglect of personal and professional responsibilities, and continued use despite harmful effects. Individuals with Percocet addiction experience persistent cravings, irritability when unable to access the drug, and increased tolerance requiring them to use higher doses over time. These signs demonstrate a psychological dependency that makes it difficult for users to control or reduce their intake.
-
Withdrawal Symptoms: Withdrawal symptoms are both physical and psychological side effects that arise when Percocet use is reduced or stopped. Physical symptoms include vomiting, chills, muscle pain, and excessive sweating, while psychological symptoms involve anxiety, irritability, restlessness, and intense cravings for the drug. These withdrawal effects highlight the body’s physical and psychological reliance on Percocet, as the absence of the drug disrupts normal functioning and increases distress. 80% of individuals who are dependent on opioids will experience withdrawal symptoms when they stop using opioids according to the Substance Abuse and Mental Health Services Administration (SAMHSA).
-
Overdose Symptoms: Overdose symptoms are physical side effects and critical signs of excessive Percocet use, presenting a life-threatening response to high doses. Symptoms of overdose include extremely slow or irregular breathing, pinpoint pupils, extreme drowsiness, blue-tinged lips or fingers (cyanosis), and potentially loss of consciousness or coma. These signs reflect the severe impact of Percocet on the central nervous and respiratory systems, as high doses depress vital functions and create an urgent need for medical intervention. In 2020, nearly 75% of all drug overdose deaths involved an opioid, showing Percocet’s role in overdose fatalities across the country according to SAMHSA.
When Does Percocet Consumption Cause Addiction?
Percocet consumption causes addiction when it is used beyond the prescribed duration or dosage. Doctors prescribe Percocet for acute pain and limit it to a maximum of 3-7 days at the lowest effective dose. For example, a standard starting dose is 5 mg of oxycodone with 325 mg of acetaminophen every 4-6 hours, not exceeding 12 tablets per day. Going beyond these guidelines, either by extending use for weeks or increasing the dose, raises the risk of addiction significantly, as it leads to physical and psychological dependency on the drug’s effects.
Men and women have different tolerance levels and risk factors in general. Men metabolize certain opioids faster, which requires slightly higher doses for the same effect, while women are more susceptible to prolonged effects, which leads to a faster development of dependency at lower doses according to “WHRY Offers Roadmap to Address Sex Differences in Opioid Epidemic” published in 2021 by Yale School of Medicine. Personal factors such as body weight, metabolism, and history of substance use also influence addiction risk, making it important to adhere strictly to prescribed guidelines.
What Is the Withdrawal Timeline for Percocet?
The withdrawal timeline for Percocet is 7 to 10 days, with symptoms beginning 6-12 hours after the last dose, peaking around 72 hours, and tapering off over 1 to 2 weeks according to MedlinePlus, a service of the U.S. National Library of Medicine. Symptoms of withdrawal generally begin 8 to24 hours after the last dose. This average timeline differs slightly based on individual factors, such as gender; studies show that women may experience withdrawal symptoms more intensely due to hormonal differences, potentially extending the discomfort by a few days.
Factors that shorten the withdrawal duration include medical detoxification, where medications are administered to alleviate symptoms, and individualized support plans that target physical and psychological symptoms. Additionally, factors such as hydration, nutrition, and emotional support during withdrawal contribute to a smoother, possibly shorter withdrawal experience.
How to Treat Percocet Addiction
To treat Percocet addiction requires a combination of medical and therapeutic approaches that address both physical dependence and psychological factors. The most effective treatment plans include a comprehensive approach incorporating medical detoxification, counseling, and support groups, along with other supportive therapies to sustain long-term recovery.
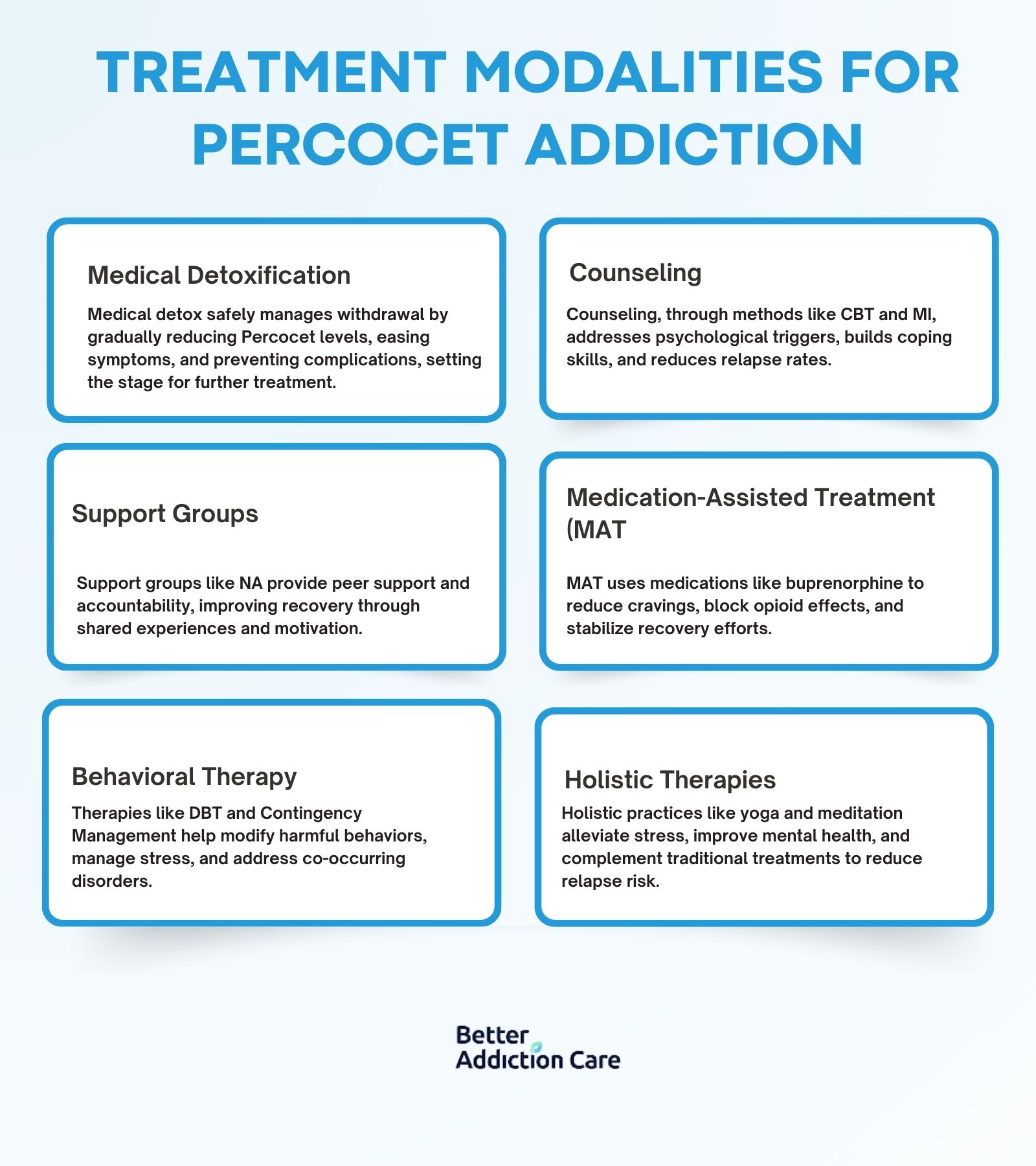
The treatment modalities for Percocet Addiction includes:
-
Medical Detoxification: Medical detox is the first step that safely manages withdrawal symptoms by gradually reducing Percocet levels under medical supervision. During detox, medications are often prescribed to ease symptoms like nausea, muscle pain, and anxiety. Medical detox is highly effective at preparing individuals for ongoing treatment by alleviating immediate physical dependency and preventing complications during withdrawal.
-
Counseling: Counseling addresses the underlying psychological triggers of Percocet addiction, such as stress, trauma, or mental health issues. Common approaches include Cognitive Behavioral Therapy (CBT) and Motivational Interviewing (MI), which help individuals develop healthier coping mechanisms. Counseling has proven effectiveness in reducing relapse rates by promoting behavioral changes and improving emotional resilience.
-
Support Groups: Support groups like Narcotics Anonymous (NA) provide a sense of community and accountability, which are important for sustained recovery. These groups offer peer support and shared experiences, helping individuals feel less isolated in their journey. Studies indicate that regular participation in support groups can significantly improve long-term recovery rates by fostering connection and motivation.
-
Medication-Assisted Treatment (MAT): MAT uses FDA-approved medications like buprenorphine or methadone to reduce cravings and block opioid effects in the brain. MAT is especially effective for managing addiction over the long term, as it lessens the likelihood of relapse and stabilizes brain chemistry, allowing individuals to focus on recovery without the overwhelming urge to use.
-
Behavioral Therapy: Behavioral therapies, such as Dialectical Behavior Therapy (DBT) and Contingency Management, provide structured approaches to modifying behaviors linked to addiction and diagnosing co-occurring mental health disorders. These therapies improve emotional regulation, problem-solving skills, and stress management, making them highly effective when combined with medical treatment in reducing relapse risk.
-
Holistic Therapies: Incorporating holistic therapies like yoga, mindfulness meditation, and exercise help support recovery by addressing stress and improving physical health. These therapies are beneficial for managing symptoms of anxiety and depression, which accompany addiction, and have shown effectiveness in reducing relapse rates when combined with conventional treatment.
How is Percocet Regulated in the US?
Percocet is regulated in the United States as a Schedule II controlled substance under the Controlled Substances Act (CSA). This classification means that while Percocet has accepted medical uses, it carries a high potential for abuse and dependency, leading to strict regulations on prescribing and dispensing. The Drug Enforcement Administration (DEA) oversees Percocet's regulation, enforcing limitations on quantities prescribed, refill restrictions, and mandatory follow-up appointments for ongoing prescriptions.
What is Percocet Used For?
Percocet is used for the relief of moderate to severe pain. It is prescribed when other pain management options are inadequate, especially for individuals experiencing pain that is unmanageable by standard analgesics. Percocet is helpful for patients who have a hypersensitivity to alternatives like ibuprofen or aspirin, as it combines oxycodone, an opioid analgesic, with acetaminophen, a non-opioid pain reliever. It is used for conditions like osteoarthritis, rheumatoid arthritis, or severe back pain that hasn’t responded well to other therapies. In some cases, patients with severe pain from endometriosis or debilitating menstrual pain or kidney stones would be prescribed Percocet when standard treatments are ineffective. Percocet is generally reserved for short term situations where other pain relievers (like NSAIDs or acetaminophen alone) are not sufficient due to its potency and potential for dependence.
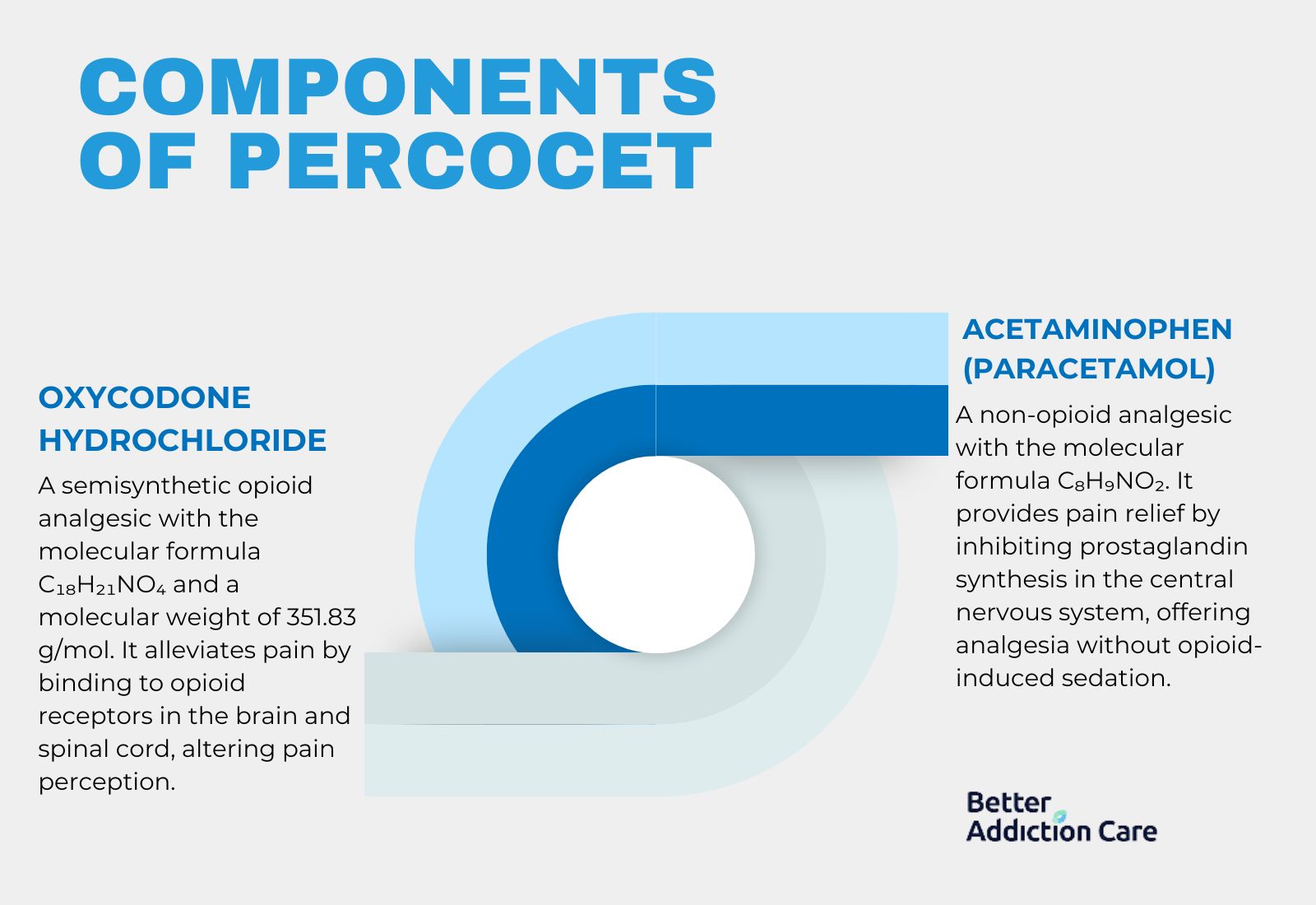
What is the Chemical Composition of Percocet?
The chemical composition of Percocet is a combination of oxycodone hydrochloride and acetaminophen, each contributing distinct analgesic effects.
-
Oxycodone Hydrochloride: This is a semisynthetic opioid with the molecular formula C₁₈H₂₁NO₄ and a molecular weight of 351.83 g/mol. Oxycodone works by binding to opioid receptors in the brain and spinal cord, altering the perception of pain.
-
Acetaminophen (Paracetamol): Represented by the molecular formula C₈H₉NO₂, acetaminophen is a widely used non-opioid analgesic. It works primarily by inhibiting prostaglandin synthesis in the central nervous system, contributing to pain relief without the sedative effects associated with opioids.
Together, these components provide a synergistic analgesic effect, making Percocet effective for pain relief in appropriate clinical scenarios.
Can You Overdose on Percocet?
Yes, you can overdose on Percocet, especially if you exceed the recommended dosage. Typical prescribed doses for Percocet range from 5 mg to 10 mg of oxycodone with 325 mg to 650 mg of acetaminophen per tablet, taken every 4 to 6 hours as needed. Taking more than this prescribed amount increases the risk of overdose. Serious, life-threatening, or fatal respiratory depression may occur with use of Percocet, especially during initiation or following a dosage increase as stated on the official drug label provided by The U.S. Food and Drug Administration (FDA).
What Happens if You Take Too Much Percocet?
If you take too much Percocet you can experience an overdose. Symptoms of overdose include slowed or labored breathing, extreme drowsiness, confusion, and even loss of consciousness. Other signs include bluish lips or skin, cold and clammy skin, low blood pressure, and pinpoint pupils. In severe cases, an overdose can result in respiratory failure, which is life-threatening and requires immediate medical intervention according to “Oxycodone and acetaminophen (oral route)” published by the Mayo Clinic. In severe cases, an overdose results in respiratory failure, which is life-threatening and requires immediate medical intervention.
Can Percocet Cause an Overdose?
Yes, Percocet can cause an overdose because it contains oxycodone, a powerful opioid. An overdose on Percocet leads to suppressed breathing and oxygen deprivation, which, if untreated, would result in coma, irreversible brain damage, or death. Additionally, acetaminophen in Percocet may cause severe liver damage when taken in high doses. Doses above 4,000 mg daily have been linked to acute liver failure, sometimes requiring transplant or resulting in death according to “PERCOCET- oxycodone hydrochloride and acetaminophen tablet.” published by DailyMed.
What is the Dosage for Percocet?
The dosage for Percocet is typically 1 tablet, 7.5 mg of oxycodone and 325 mg of acetaminophen, every 6 hours, however it varies by formulation. General guidelines apply to both male and female adults but specific factors like body weight, metabolism, and pain tolerance influence a provider’s recommendation.
The standard adult dosages for each formulation of Percocet is written below:
-
Percocet 5 mg/325 mg:
-
Male: Up to 2 tablets every 6 hours, not to exceed 12 tablets (or 60 mg oxycodone and 3,900 mg acetaminophen) in 24 hours.
-
Female: Up to 2 tablets every 6 hours, with a similar daily maximum of 12 tablets. Women with lower body weights require monitoring to avoid excessive sedation or respiratory effects.
-
Percocet 7.5 mg/325 mg:
-
Male: 1 tablet every 6 hours, not to exceed 8 tablets (or 60 mg oxycodone and 2,600 mg acetaminophen) per day.
-
Female: 1 tablet every 6 hours with a maximum of 8 tablets per day. Dosage adjustments should be considered in females with slower metabolism to avoid side effects.
-
Percocet 10 mg/325 mg:
-
Male: 1 tablet every 6 hours, with a daily limit of 6 tablets (or 60 mg oxycodone and 1,950 mg acetaminophen).
-
Female: 1 tablet every 6 hours, not exceeding 6 tablets per day. Lower doses or less frequent intervals are advised for females sensitive to opioids.
For both males and females, exceeding 4,000 mg of acetaminophen in 24 hours risks liver damage, while keeping total oxycodone intake within prescribed limits helps avoid dependency and overdose risks.
Does Percocet Treat Opiate Withdrawal?
No, Percocet does not treat opiate withdrawal. Percocet is specifically designed for pain relief, not for managing withdrawal symptoms. Using Percocet for withdrawal leads to further dependency due to its oxycodone content, which is a habit-forming opioid. Additionally, medications like methadone or buprenorphine are recommended over Percocet for managing opioid withdrawal safely and effectively.
Does Percocet Make You High?
Yes, Percocet makes you high because it contains oxycodone, an opioid that activates the brain’s reward pathways, leading to euphoria. The euphoric effects amplify when taken in higher-than-prescribed doses, which is why some misuse it recreationally. The acetaminophen component does not reduce these effects, allowing the oxycodone to act directly on the central nervous system.
Is Percocet a Narcotic?
Yes, Percocet is a narcotic because it contains oxycodone, a controlled opioid that affects the central nervous system and carries a high potential for misuse and dependency. Narcotics are a class of drugs that act on the central nervous system to relieve pain, induce sleep, and produce feelings of euphoria. Opioids, including oxycodone, fall under the narcotic classification due to their powerful pain-relieving properties and risk for dependency and abuse according to the National Institute on Drug Abuse (NIDA).
Is Percocet a Benzodiazepine?
No, Percocet is not a benzodiazepine because it is classified as an opioid pain reliever rather than an anti-anxiety medication. Unlike benzodiazepines, which work on the central nervous system to produce sedative effects by enhancing GABA neurotransmitters, Percocet combines oxycodone and acetaminophen to specifically target pain relief. The primary purpose of benzodiazepines is to manage anxiety, insomnia, or seizures, while Percocet is prescribed for moderate to severe pain management. Benzodiazepines and opioids act on different receptors in the brain: benzodiazepines on GABA receptors, while opioids like oxycodone target opioid receptors to relieve pain.
Does Percocet Interact With Other Medications?
Yes, Percocet interacts with other medications including other opioids, benzodiazepines, antidepressants, gabapentin, and alcohol.The number of overdose deaths involving opioid painkillers rose from approximately 4,000 in 1999 to over 16,000 in 2010. Many of these overdoses involved additional drugs or alcohol according to The U.S. Department of Health and Human Services.
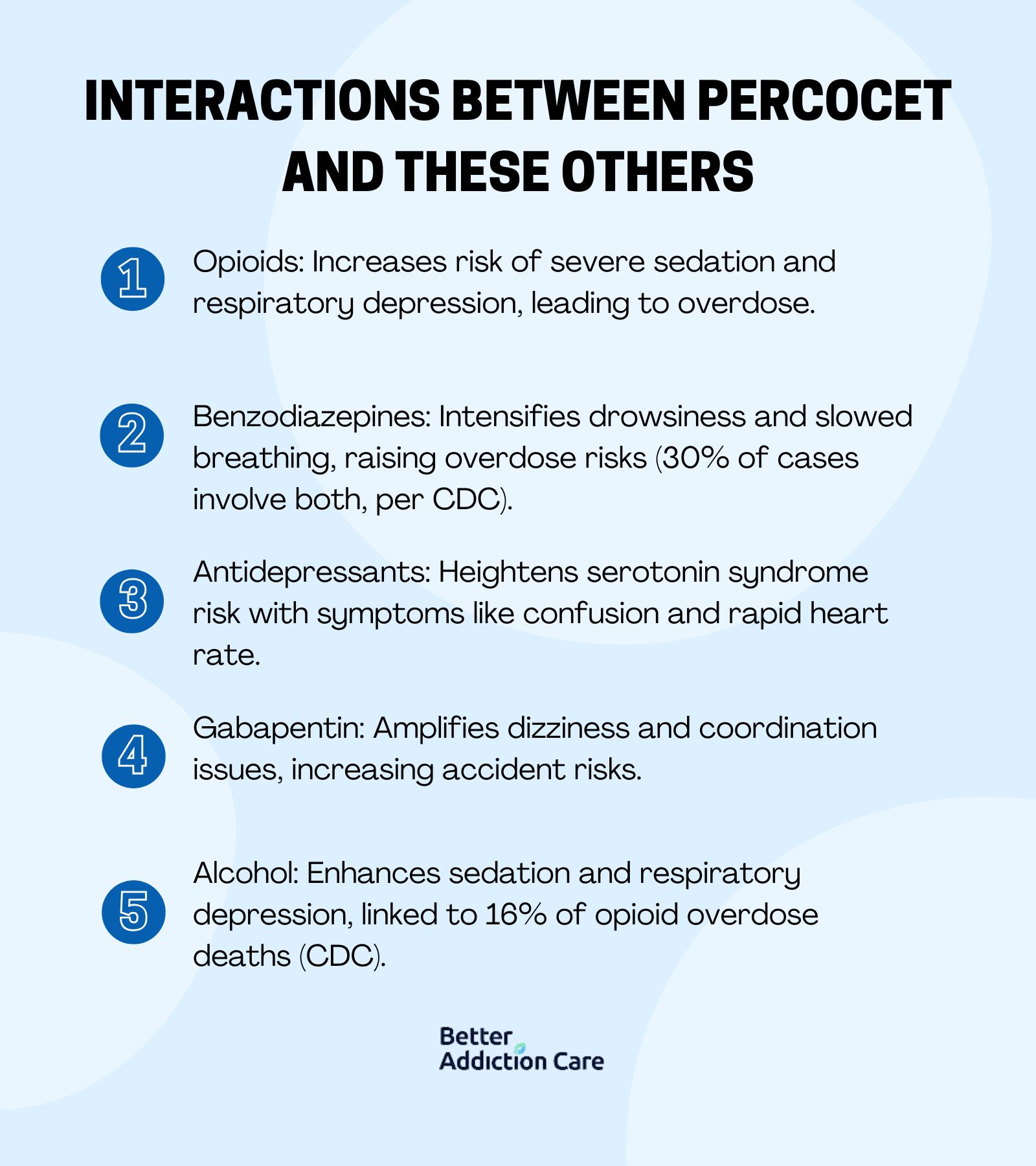
The interactions between Percocet and these other substances are listed below:
-
Opioids: Combining Percocet with other opioids, like morphine or codeine, raises the risk of severe respiratory depression and sedation, potentially leading to overdose.
-
Benzodiazepines: When taken with benzodiazepines (e.g., Xanax or Valium), Percocet causes intense drowsiness and significantly slowed breathing, increasing the risk of coma and overdose. An analysis of overdose deaths showed that in cases involving prescription opioids like Percocet, approximately 30% also involved benzodiazepines according to the Centers for Disease Control (CDC)
-
Antidepressants: Using Percocet with SSRIs or MAOIs heightens the risk of serotonin syndrome, a dangerous condition affecting the nervous system with symptoms like confusion, rapid heart rate, and high blood pressure.
-
Gabapentin: Taking gabapentin alongside Percocet amplifies side effects such as dizziness, drowsiness, and coordination issues, raising the risk of falls and other accidents.
-
Alcohol: Alcohol intensifies Percocet’s sedative effects, further impairing motor skills and alertness. This combination risks life-threatening respiratory depression and overdose. Alcohol was linked to approximately 16% of opioid-related overdose deaths in 2020 and 2021, showing how dangerous this combination can be due to amplified respiratory depression effects from both substances according to the CDC.
Is Percocet a Strong Muscle Relaxer?
No, Percocet is not a strong muscle relaxer because it is specifically designed to relieve pain rather than relax muscles. It targets pain receptors in the brain to reduce the perception of pain, rather than directly impacting muscles. Unlike muscle relaxers, which reduce muscle spasms by acting on specific receptors in the central nervous system or peripheral muscles, Percocet’s primary mechanism does not alleviate muscle tension. While Percocet may offer some general relaxation due to its opioid content, this effect is not comparable to the direct muscle relaxation provided by medications like cyclobenzaprine or methocarbamol. Increasing the dosage of Percocet would enhance pain relief but does not change its limited effect on muscle relaxation.
Is Percocet a Strong Painkiller?
Yes, Percocet is a strong painkiller because its main component is oxycodone, an opioid that binds to receptors in the brain and spinal cord to block pain signals, which provides substantial relief for moderate to severe pain. Acetaminophen, the second component, adds to the analgesic effect by reducing inflammation and fever, supporting the overall pain relief. The effectiveness of Percocet does increase with a higher dosage of oxycodone, as it offers stronger pain relief, but this also raises the risk of side effects and dependency.
What is the Difference Between Percocet and Vicodin?
The difference between Percocet and Vicodin is their active ingredients and effects. Percocet contains oxycodone and acetaminophen, while Vicodin combines hydrocodone and acetaminophen, according to Pope, C 2023 in “Vicodin vs Percocet: What's the difference?”on Drugs.com. Oxycodone in Percocet is more potent than hydrocodone in Vicodin, making Percocet slightly stronger in pain-relief effects and potentially more addictive. Both medications are opioids, meaning they carry a risk of addiction, but the higher potency of oxycodone may lead to a faster development of dependence in Percocet users.
Both medications are prescribed for moderate to severe pain and share common side effects like drowsiness, nausea, and constipation. Chemically, oxycodone is known as C₁₈H₂₁NO₄, while hydrocodone is C₁₈H₂₁NO₃, and acetaminophen in both is C₈H₉NO₂.
Does Percocet Make You Tired?
Yes, Percocet does make you tired because it contains oxycodone. Oxycodone binds to opioid receptors in the brain, producing sedative effects and reducing overall brain activity, which leads to drowsiness and fatigue. Additionally, the pain-relieving properties of Percocet induce a sense of relaxation, further contributing to tiredness. Individuals who misuse Percocet experience significant fatigue, leading to feelings of sleepiness or weakness. This drowsiness can interfere with daily activities like driving or engaging in potentially dangerous tasks according to Casarella, J. 2022 in “Dealing with Side Effects of Percocet” published by WebMD.
Is Percocet a Controlled Drug?
Yes, Percocet is a controlled drug. Percocet is classified as a Schedule II controlled substance in the United States, indicating that it has a high potential for abuse and dependence. As an opioid analgesic, Percocet is also subject to the Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS), a program designed to ensure safe prescribing and use due to the associated risks of addiction and overdose.
What Are the Types of Percocet Pills?
The types of Percocet pills include formulations that vary in the strength of oxycodone, such as 2.5 mg, 5 mg, 7.5 mg, and 10 mg. Each of these strengths is combined with 325 mg of acetaminophen. The different dosages represent varying levels of pain relief, allowing healthcare providers to tailor treatments based on the severity of a patient’s pain. No commonly available Percocet formulations exist beyond these strengths, ensuring a consistent approach to managing moderate to severe pain while minimizing risks associated with opioid use.
Related Articles
Treatment Centers in Georgia









