Pristiq Withdrawal: Symptoms, Timeline, and Care
When Pristiq levels drop abruptly, serotonin and norepinephrine signaling changes suddenly, and the nervous system struggles to maintain balance. This internal shift can create physical sensations, mood changes, and sleep disruptions.

Key Takeaways
-
Is Pristiq withdrawal real? → Yes. It’s temporary, common, and usually manageable with proper support. It’s simply your brain readjusting after the medication.
-
What’s the safest way to stop? → A slow, doctor-guided taper helps minimize symptoms and keeps you stable. Adjusting the pace makes the transition much smoother.
-
What supports recovery? → Steady routines, emotional support, and healthy habits make the process easier and more comfortable. Small daily steps can significantly ease how you feel.
What Pristiq Is and How It Works?
Pristiq (desvenlafaxine) is an SNRI; serotonin-norepinephrine reuptake inhibitor. It is most commonly prescribed for major depressive disorder. It works by increasing the availability of two essential neurotransmitters: serotonin, which supports emotional stability, and norepinephrine, which regulates energy, focus, and stress response.
When someone takes Pristiq consistently, the brain adapts to these steady levels of neurotransmitters. Over time, neural circuits adjust their sensitivity and activity in response to the medication. This doesn’t mean dependence in the addictive sense; it’s simply the brain learning to work with the chemical support it’s been given. [1]
Because of this adaptation, stopping Pristiq too quickly can feel like suddenly removing a stabilizing beam from a building. The structure is still strong, but it needs time to redistribute weight and find equilibrium again. That adjustment period is what we recognize as withdrawal.
Why Withdrawal Happens?
Withdrawal happens because the brain needs time to recalibrate. When Pristiq levels drop abruptly, serotonin and norepinephrine signaling changes suddenly, and the nervous system struggles to maintain balance. This internal shift can create physical sensations, mood changes, and sleep disruptions.
These reactions do not occur because the medication is “addictive.” They occur because the body has become accustomed to a predictable chemical environment, and rapid shifts create temporary discomfort. It’s very similar to what happens when someone adjusts to a new sleep schedule or transitions to a different climate—the body can adapt, but it does so gradually.
The intensity of withdrawal varies widely. Some people barely notice it. Others feel a strong wave of symptoms that can be distressing—not dangerous, but deeply uncomfortable. Learning what to expect helps individuals move through the process with more confidence and less fear.
Withdrawal vs. Relapse
One of the hardest parts of Pristiq withdrawal is telling the difference between withdrawal symptoms and the return of depression. The two can look similar, especially during the first two weeks of tapering. This is where clear guidance and emotional support matter.
Withdrawal symptoms are usually short-lived, unpredictable, and often accompanied by physical sensations like dizziness or brain zaps. [2] They tend to improve as the body adjusts to each new dose. Relapse, on the other hand, typically appears more gradually and reflects the return of persistent depressive thinking—not sudden shifts.
Understanding this difference helps people stay grounded. Experiencing irritability or low mood during withdrawal doesn’t mean they’re “back to square one.” It means their brain is adjusting. With patience and support, withdrawal symptoms pass, and real healing continues.
What Are the Common Symptoms of Pristiq Withdrawal?
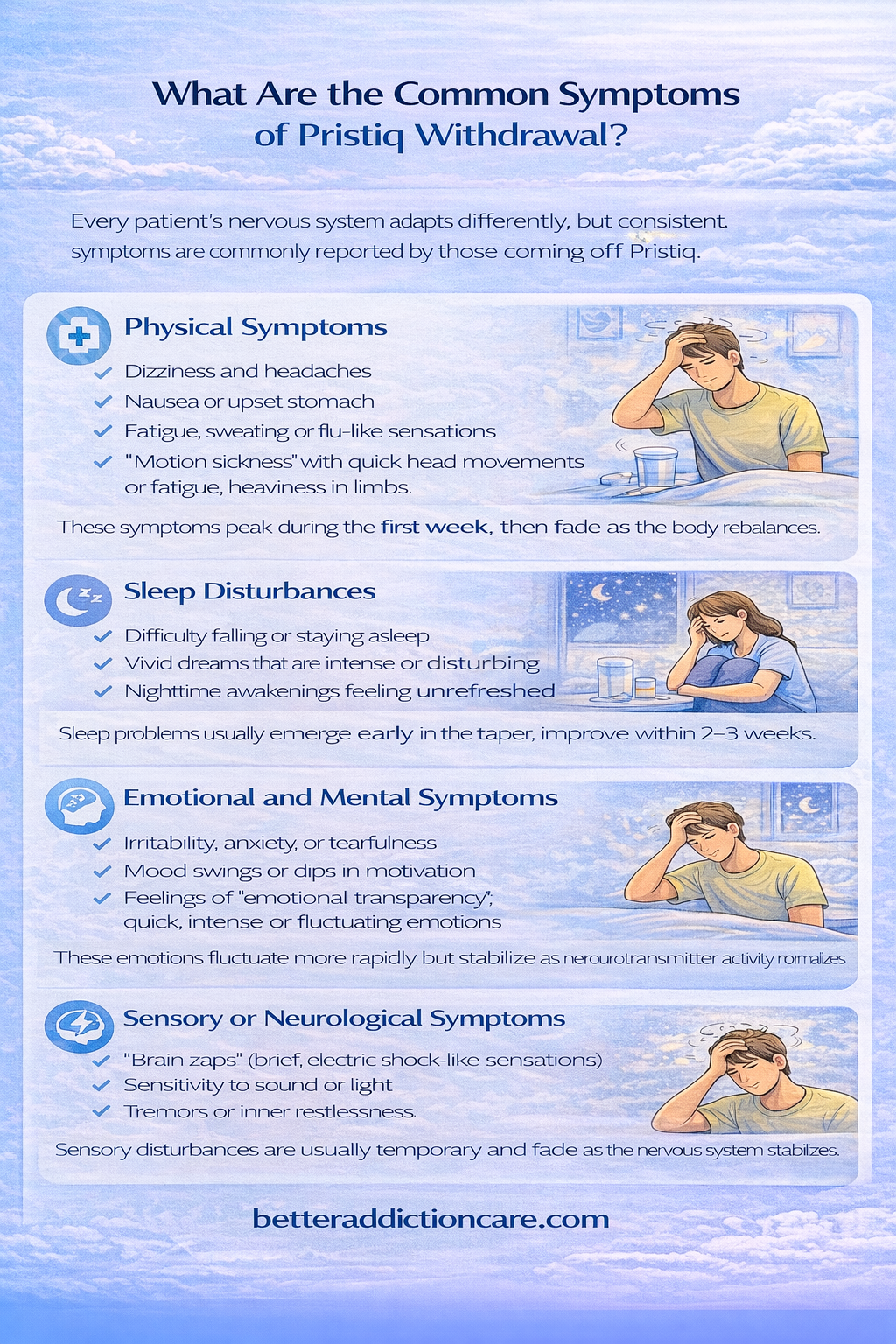
Physical Symptoms
Physical withdrawal symptoms from Pristiq can include dizziness, headaches, nausea, fatigue, sweating, and flu-like sensations. Some people feel a sudden sense of “motion sickness,” especially when turning the head or moving quickly. Others describe a heaviness in the limbs or a sudden drop in energy that makes normal tasks feel more draining.
These physical sensations are uncomfortable, but they’re also temporary. They reflect the body recalibrating neurotransmitter levels and adjusting to new neural activity. Most symptoms peak within the first week, then gradually fade as levels stabilize.
Gentle reassurance is important here: these physical experiences are not signs of harm. The body is doing exactly what it needs to do to restore balance. Staying hydrated, eating regularly, and resting when necessary can make the process much easier.
Sleep Disturbances
Sleep disruptions are one of the most common and distressing withdrawal effects. People may have trouble falling asleep, staying asleep, or reaching deep, restful sleep. Others experience vivid dreams or frequent nighttime awakenings that make mornings feel heavy and unrefreshed.
These sleep symptoms typically appear within the first few days of tapering and often peak around the end of week one. Improvement usually begins during weeks two or three as neurotransmitter levels stabilize. Sleep gradually becomes more predictable, and the body begins to feel rested again.
Having a consistent evening routine—dimming lights, reducing screen time, and engaging in calming practices—can support the brain as it relearns its natural sleep rhythms.
Emotional and Mental Symptoms
Emotional changes during Pristiq withdrawal can include irritability, anxiety, tearfulness, restlessness, and sudden mood swings. Some people describe feeling “emotionally transparent,” where feelings arrive quickly and strongly. Others feel a temporary dip in motivation or interest.
These emotional symptoms often mimic depression, which can understandably cause confusion or fear. But there’s an important distinction: withdrawal emotions tend to appear suddenly and fluctuate rapidly.
They’re not the slow, persistent return of depressive thinking. They are short-term neurochemical responses that fade as the taper progresses.
Being gentle with oneself during this phase is crucial. Emotional volatility doesn’t mean personal failure—it means the brain is healing.
Sensory or Neurological Symptoms
“Brain zaps” are perhaps the most recognized and feared withdrawal symptom. These are brief, electrical-shock sensations in the head or body, often triggered by eye movement or sudden turns. [2] Although startling, they are not dangerous.
Other neurological symptoms can include sensitivity to light or sound, tremors, or a sense of inner restlessness. These are less common but entirely temporary as the nervous system recalibrates its signaling pathways.
These symptoms are often the last to resolve but improve significantly as the taper slows and stabilizes.
What Is the Typical Pristiq Withdrawal Timeline?
Days 1–3: Early Adjustment Phase
During the first few days after reducing the dose, the body begins noticing the shift in neurotransmitter levels. Symptoms may be mild at first—slight dizziness, increased yawning, or mild nausea. Some individuals report feeling “off-center” but still functional.
Sleep may begin changing in this early phase, with either fatigue or restlessness emerging. Emotions can also fluctuate more easily. This period is usually manageable but signals the beginning of the adjustment process.
Weeks 1–2: Peak Discomfort
This is when withdrawal tends to feel the most intense. Physical symptoms like dizziness, headaches, nausea, and fatigue may peak. Emotional volatility—anger, anxiety, sadness—can become more noticeable. People often describe this phase as “riding waves,” with periods of discomfort followed by brief moments of relief.
Sleep disruptions often intensify here. Insomnia, vivid dreams, or early-morning awakenings are common. The nervous system is working hard to stabilize, and the body is using significant energy to adapt.
This period can feel overwhelming, but it is also temporary. Most people begin to notice gradual shifts toward improvement at the end of week two.
Weeks 3–4: Improvement Phase
By the third and fourth week, many symptoms begin easing. Physical sensations lighten, energy becomes more stable, and the emotional intensity softens. Sleep patterns begin normalizing, and mornings feel less foggy.
This phase is often encouraging. People begin recognizing their own emotions more clearly without the interference of withdrawal. Motivation and focus begin returning, and the body feels stronger.
One Month and Beyond: Adjustment Phase
After a month, many people feel significantly better, but some may continue experiencing occasional “echoes” of withdrawal—mild dizziness, emotional waves, or brief sleep disturbances. These lingering effects are normal and tend to fade gradually.
The brain is still fine-tuning neurotransmitter pathways during this time. A consistent routine, nourishing habits, and ongoing support help cement long-term stability.
Why Timelines Differ
No two withdrawal journeys look exactly alike. Factors that influence the timeline include dosage, how long Pristiq was taken, tapering speed, overall health, stress levels, and individual brain chemistry. [3] Some people recover quickly; others need a slower pace.
The important thing is not comparing to others but working with your provider to tailor a taper that fits your body’s needs.
Why Should Pristiq Be Tapered Slowly?
Risks of Quitting Cold Turkey
Stopping Pristiq abruptly can cause intense withdrawal symptoms—severe dizziness, nausea, insomnia, emotional crashes, panic, or overwhelming irritability.
Cold turkey increases the risk of confusion between withdrawal and relapse, leaving people unsure whether their symptoms reflect healing or regression.
Rapid discontinuation also increases the risk of “rebound depression,” which is not the return of the original illness but a temporary neurochemical crash caused by sudden medication removal.
Benefits of a Gradual Taper
A gradual taper allows the brain to adjust slowly to each reduction in dose. This leads to gentler symptoms, better sleep, and a more stable mood. People often feel more in control and more connected to their own emotional patterns when the process is paced thoughtfully.
Slow tapering also reduces the likelihood of prolonged withdrawal, making recovery more predictable and sustainable.
Key Principle — “Go Slow to Go Steady”
Tapering should be built around the individual, not the calendar. Providers often adjust the schedule based on how each reduction feels. The safest and most effective approach is flexible, patient, and responsive to the body’s signals.
How Healthcare Providers Support Pristiq Withdrawal?

Monitoring Symptoms and Adjusting Taper Speed
A provider’s role is to create a taper plan that respects your nervous system. They track symptoms, monitor energy levels, and assess emotional changes.
If symptoms become overwhelming, your provider can slow the taper, pause it, or slightly increase the dose before continuing at a gentler pace.
This personalized pacing makes the process safer and more humane.
Distinguishing Withdrawal From Relapse
Mental health providers help differentiate between temporary withdrawal effects and genuine changes in mood or functioning. This clarity prevents unnecessary fear and helps individuals stay committed to the taper with confidence.
Temporary Medications or Interventions
Short-term aids for sleep, nausea, or anxiety may be offered during the taper. These are not long-term solutions but supportive tools to make the transition easier. Providers may also recommend supplements, specific therapies, or lifestyle adjustments tailored to individual needs.
Ongoing Mental Health Monitoring
Regular follow-ups create an essential safety net. These check-ins help identify patterns, track progress, and address challenges early. Providers also support long-term wellness by encouraging habits that protect mood and emotional well-being beyond medication.
Coping Strategies That Help During Pristiq Withdrawal
Improving Sleep Quality
Sleep problems during withdrawal are common but manageable. Establishing a calming pre-sleep routine helps signal to the brain that it is safe to rest. This might include dimming lights, practicing deep breathing, or reading something soothing.
Avoiding heavy meals, caffeine, and bright screens in the evening supports melatonin production and reduces nighttime restlessness. [4] If sleep remains difficult, grounding exercises or gentle nighttime stretches can calm an overactive nervous system.
What to Eat and Drink During Withdrawal
Stable blood sugar can significantly improve withdrawal symptoms. Meals that include protein, healthy fats, and complex carbohydrates provide steady energy and reduce irritability.
Magnesium-rich foods—leafy greens, nuts, legumes—support relaxation and muscle function.
Hydration is equally crucial. Even mild dehydration can worsen dizziness, fatigue, and headaches. Avoiding sugary drinks and limiting energy drinks or heavy caffeine prevents crashes that amplify withdrawal discomfort.
Gentle Exercise and Movement
Movement helps the body regulate stress hormones and improves mood. During withdrawal, heavy exercise may feel overwhelming, but gentle activities like walking, stretching, yoga, or light strength training can improve energy and sleep.
Exercise also increases the production of endorphins—natural mood stabilizers that support emotional resilience during tapering.
Reducing Stress and Anxiety
Withdrawal can heighten stress sensitivity. Simple tools like breathing exercises, grounding techniques, progressive muscle relaxation, or journaling can help manage overwhelming moments.
Therapy—especially CBT or supportive counseling—can offer coping strategies, emotional validation, and a safe space to process feelings. Mindfulness practices also help regulate nervous system activity.
Staying Connected and Supported
Isolation makes withdrawal harder. Staying connected to a partner, family member, friend, or support group provides emotional grounding. Many people find it helpful to let at least one trusted person know they’re tapering, so they have someone to reach out to during tough days.
Connection reinforces resilience and reduces the emotional weight of the process.
Why Daily Routine Matters?
Routine acts as an anchor for the brain during withdrawal. Consistent sleep times, regular meals, morning light exposure, and predictable daily activities help regulate mood, hormones, and energy.
A steady routine supports the nervous system, reduces anxiety, and gives the brain clear signals as it adjusts to life without Pristiq.
When Should I Seek Medical Help During Withdrawal?
Some symptoms require immediate professional attention, including:
-
Suicidal thoughts or intense hopelessness
-
Severe or worsening depression
-
Persistent panic attacks
-
Extreme dizziness that affects mobility
-
Inability to sleep for several days in a row
-
Hallucinations or severe confusion
-
Any symptom that feels dangerous or unmanageable
These signs don’t mean something irreversible is happening—they signal that you need more support or a slower taper.
When Symptoms Don’t Improve?
If symptoms remain intense beyond a few weeks or keep interfering with daily functioning, your provider may adjust your taper plan. This might involve slowing reductions, pausing the taper, or temporarily raising the dose.
The goal is not speed—it’s stability and safety.
What Comes After Withdrawal? (Long-Term Recovery)
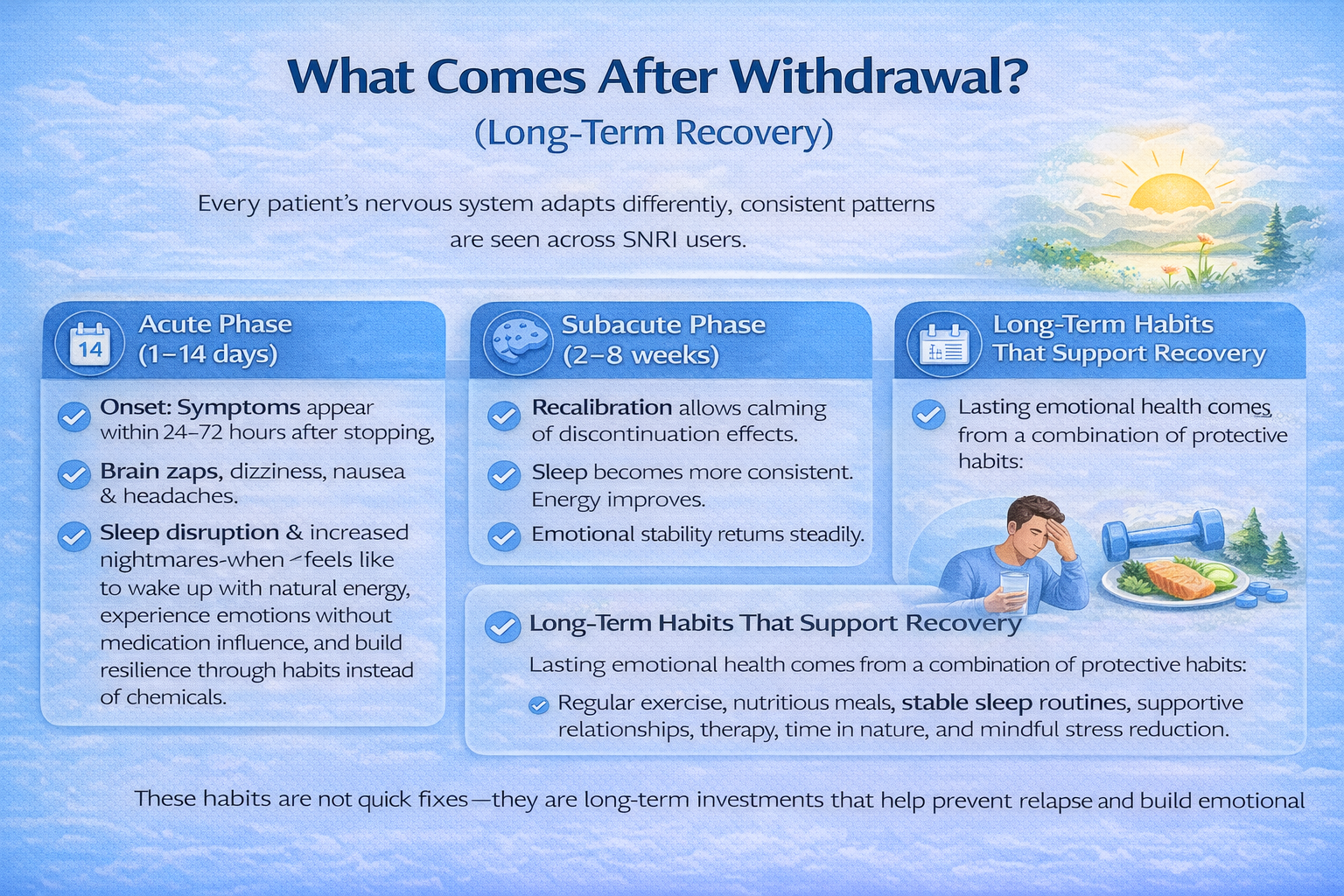
Rediscovering Your Natural Rhythm
Once Pristiq is fully discontinued, the brain gradually settles into its natural rhythm. Mood becomes more predictable, emotional range widens, and daily life feels more grounded. [5] This phase often brings a sense of rediscovery—what it feels like to wake up with natural energy, experience emotions without medication influence, and build resilience through habits instead of chemicals.
Importance of Follow-Up Appointments
Even after withdrawal symptoms fade, follow-up appointments matter. They help monitor mood, track long-term patterns, and ensure that support remains accessible. Providers also help patients build strategies for maintaining well-being without medication.
Long-Term Habits That Support Recovery
Lasting emotional health comes from a combination of protective habits:
Regular exercise, nutritious meals, stable sleep routines, supportive relationships, therapy, time in nature, and mindful stress reduction.
These habits are not quick fixes—they are long-term investments that help prevent relapse and build emotional resilience.
Conclusion
Pristiq withdrawal can be uncomfortable, but it is also temporary and manageable. With a slow taper, consistent medical guidance, and healthy daily habits, most people move through this transition successfully. The brain has a remarkable ability to heal and rebalance when given time, patience, and support.
Withdrawal is not a setback—it’s a phase of recovery. You are not failing; you are adjusting. And with the right care, you can move forward with stability, clarity, and renewed confidence.
FAQs
It’s strongly discouraged. Stopping abruptly increases withdrawal risk and can trigger severe symptoms.
Most symptoms peak within 1–2 weeks and steadily improve over 3–4 weeks. Some mild lingering effects may last longer but continue to fade.
Withdrawal symptoms can mimic relapse, but they are temporary. Ongoing habits and follow-ups help determine what’s withdrawal and what’s emotional baseline.
Regular meals, hydration, gentle movement, a calming routine, and stress-management tools significantly reduce discomfort.
By offering patience, checking in, helping with daily tasks when needed, and being emotionally present during tough moments.
Reach out to your provider. A slower taper or brief medication adjustments can make the process safer and more tolerable.







