Is Seroquel (Quetiapine) Addictive? Symptoms, Uses & Side Effects
Seroquel is the brand name for quetiapine, a type of atypical antipsychotic first approved in the late 1990s.
It works by blocking certain brain receptors, mainly serotonin and dopamine, which helps balance mood and thoughts. It also has strong sedating effects because it affects histamine and noradrenaline.
Clinically, quetiapine is prescribed for:
-
Schizophrenia (adults and some adolescent groups).
-
Acute manic or mixed episodes in bipolar disorder and maintenance therapy for bipolar disorder.
-
Adjunctive therapy for major depressive disorder when first-line antidepressants are insufficient.
Key Takeaways
-
Quetiapine misuse and addiction can develop gradually. It often starts with taking the medication for relief, then tolerance builds, leading to dependence and, in some cases, problematic use.
-
Misuse is not a weakness — it results from a mix of biology, mental health, and environmental factors.
-
Recovery is possible. Medical guidance, counseling, and healthy coping strategies can support safe use, reduce reliance on quetiapine, and improve long-term well-being.
Seroquel comes in immediate-release (IR) and extended-release (XR) forms. They absorb differently in the body, which changes how fast the effects start, when side effects appear, and may even influence how some people misuse it.
-
Tolerance — needing larger doses to achieve the same physiological/mood effects. With quetiapine, tolerance to sedative effects can develop in some people, but this is not the same as the reinforcing tolerance seen with addictive drugs.
-
Dependence — physiologic adaptations that cause symptoms when the drug is abruptly stopped. Quetiapine can produce discontinuation symptoms after prolonged use, which reflect dependence in the narrow physiologic sense.
-
Addiction — a syndrome of compulsive use despite harm, craving, and drug-seeking driven by reward circuitry changes. Quetiapine is not classically addictive in that it does not consistently produce euphoria and robust dopamine-mediated reinforcement; however, behavioral misuse and diversion are clinically important and documented.[1]
Signs & Symptoms Of Quetiapine Misuse
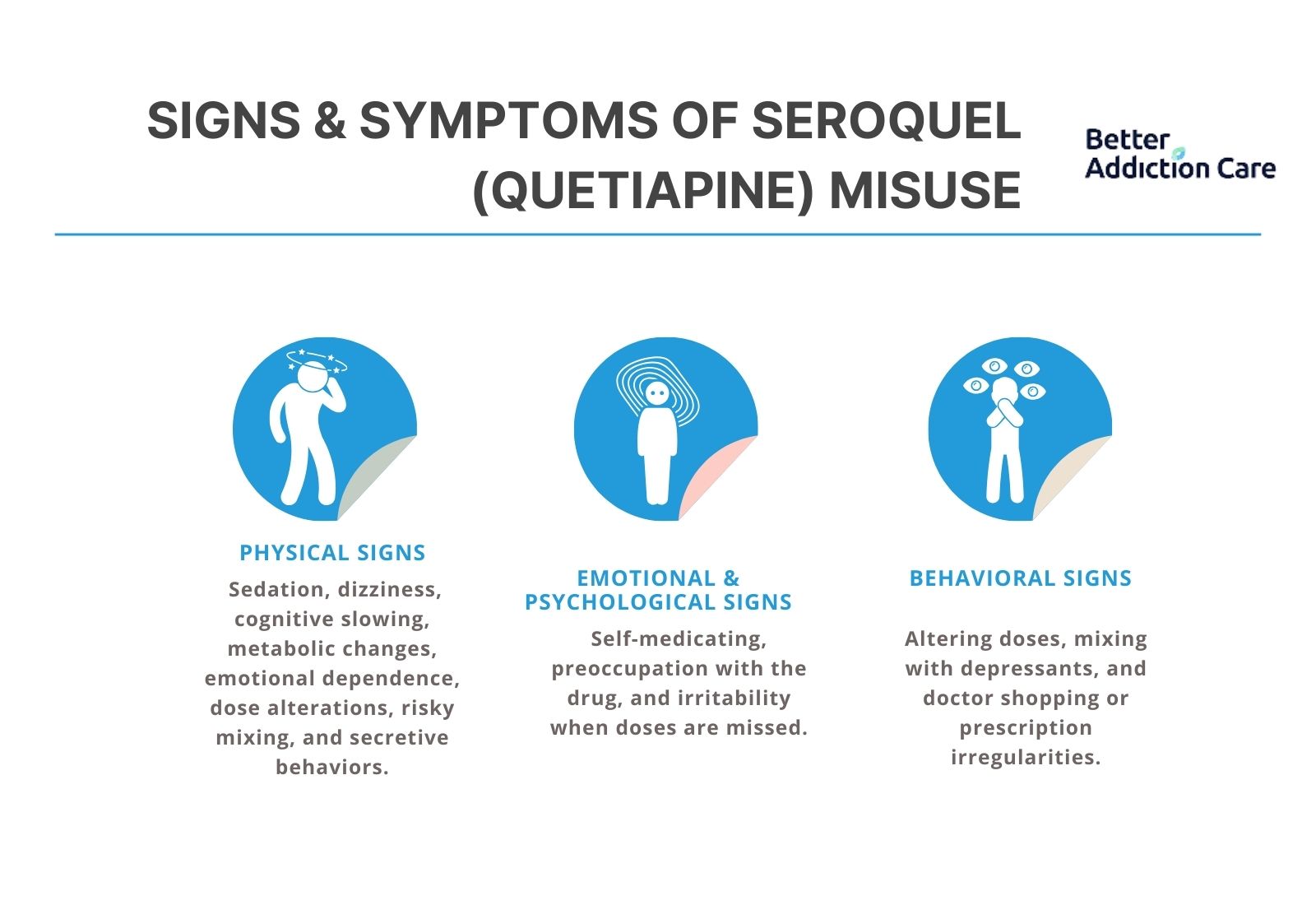
Misuse patterns with quetiapine are often behavioral and subtle. People typically do not “get hooked” the way they do on opioids, but misuse can still cause significant harm.
Physical Signs Of Misuse Or Overuse
1. Excessive Sedation or Daytime Sleepiness
Taking extra doses for sleep or using more than prescribed can make a person unnaturally drowsy during the day. They may fall asleep suddenly, feel “drugged,” or struggle to stay alert. This usually reflects improper dosing, not addiction.
2. Dizziness, Faintness, or Falls
Using too much Seroquel can drop blood pressure too low, especially when standing up. People may feel light-headed, unsteady, or even faint. Older adults are at higher risk of falls when doses are misused or “stacked.”
3. Slowed Thinking and Poor Coordination
Overuse can cause a noticeable slowdown in reaction time and mental processing. Someone may seem spacey, confused, or clumsy. This increases the risk of accidents, especially while driving or doing physical tasks.
4. Metabolic Changes
Using high doses or taking Seroquel long-term can lead to weight gain, higher blood sugar, and cholesterol changes. These shifts happen gradually and often signal that the medication is being used more heavily than intended.
5. Nausea, Sweating, Tremor, or Palpitations
Stopping Seroquel suddenly or taking too much at once can trigger uncomfortable physical symptoms. People may feel shaky, sweaty, nauseated, or notice a racing heart. These symptoms reflect discontinuation or overdose, not addiction.
Emotional & Psychological Signs
1. Using Seroquel for Self-Medication
Some people start relying on Seroquel to calm anxiety, fall asleep, or “take the edge off,” even when they don’t have a medical reason to use it. This pattern often signals misuse rather than prescribed treatment.
2. Preoccupation With the Medication
A person may become unusually focused on keeping a supply of Seroquel, worrying about running out, or using it to boost the effects of alcohol or other drugs. This preoccupation shows the medication is being used in a way it wasn’t intended.
3. Irritability or Restlessness When a Dose Is Missed
Missing a dose can lead to irritability, poor sleep, or a dip in mood. These changes often come from rebound symptoms or discontinuation effects, but people sometimes mistake them for cravings. This can reinforce a cycle of misuse.
Behavioral Signs
1. Taking Higher or Altered Doses Without Medical Guidance
Some people increase their dose on their own, split or crush tablets to make the effects kick in faster, or use someone else’s prescription. These behaviors show the medication is not being used safely or as directed.
2. Mixing Seroquel With Alcohol or Other Sedatives
Using Seroquel alongside alcohol, benzodiazepines, or sleep aids to “enhance the calm” is a major red flag. This combination can dangerously slow breathing and heart function and often signals intentional misuse.
3. Doctor Shopping or Pharmacy Irregularities
While less common than with controlled substances, some individuals may seek extra prescriptions from multiple doctors or pharmacies. Sudden changes in refill patterns or frequent “lost medication” reports can also indicate misuse.
How Common Is Quetiapine Misuse?
Quetiapine is one of the most frequently prescribed second-generation antipsychotics, and because it’s widely used, case reports and surveillance data show rising instances of misuse and diversion — particularly in emergency departments and forensic settings. However, the absolute risk of developing an addictive, drug-seeking pattern is lower than for classic substances of abuse.
General Prevalence:
A 2023 U.S. national survey found that about 6.3% of adults aged 18–59 who had used quetiapine reported misusing it in some way. [2] Misuse was often for sleep, anxiety relief, or to enhance the effects of other substances. Most cases reflect attempts at self-medication rather than true addictive behavior.
Clinical Settings:
In clinical practice, quetiapine prescribing errors are common. A 2022 chart review at a large academic medical center found that 67% of quetiapine prescriptions were considered inappropriate — wrong dose, indication, or frequency. [3]
These errors are especially risky for patients with multiple chronic conditions, newly diagnosed psychiatric disorders, or older adults who may have trouble managing medications. Such patterns reflect misunderstanding or inconsistent use, not compulsive drug-seeking.
Withdrawal Frequency:
Clinical trials of extended-release quetiapine show that 12.1% of patients experience discontinuation symptoms after abrupt cessation, compared with 6.7% of placebo patients. [4] These effects — such as insomnia, anxiety, nausea, or palpitations — are classified as physiologic discontinuation symptoms, not true addictive withdrawal. Careful tapering can usually prevent or minimize these symptoms.
Causes: Why Does Quetiapine Get Misused?

Misuse is usually behavioral and context-driven rather than driven by classic pharmacologic reinforcement.
Neurobiology (How Quetiapine Affects the Brain?)
Quetiapine works by blocking dopamine, serotonin, histamine, and adrenergic receptors, creating strong calming and sedative effects. These effects slow down overactive pathways, reduce agitation, and help with sleep, which is why some people begin misusing it. [5]
How Quetiapine Interacts With Brain Pathways?
Quetiapine:
-
Does not directly stimulate the brain’s reward system
→ No classic “euphoric high” like opioids or stimulants. -
Does not cause large dopamine spikes
→ Less risk of traditional addiction, but sedation can still feel emotionally reinforcing. -
Does not produce tolerance in the reward circuitry
→ Dose escalation happens for sedation, not for pleasure. -
Does not trigger compulsive drug-seeking through reward loops
→ Misuse is usually tied to sleep, anxiety, or emotional numbing.
Quetiapine acts like a powerful sedative switch for the nervous system — not a drug that activates pleasure pathways, but one that temporarily “turns off” stress and arousal. That calming effect is what people often start chasing.
Genetic & Biological Factors
Even though quetiapine is not addictive in the classic sense, certain biological traits can increase the likelihood of misuse:
-
Family history of substance misuse or mental illness: Increases vulnerability to using medication as a coping tool.
-
Metabolism differences: Slow metabolizers may feel stronger sedation, making the drug more reinforcing.
-
Chronic insomnia or anxiety: People with long-term sleep or stress issues may rely on quetiapine more heavily.
-
Younger adults with impulsivity traits: Higher risk of taking more than prescribed.
-
High sensitivity to emotional distress: Individuals who quickly feel overwhelmed may use quetiapine for rapid calming.
Co-occurring conditions like PTSD, bipolar disorder, depression, panic disorder, or ADHD significantly increase misuse risk because the sedating effect feels like instant relief.
Psychological & Emotional Triggers
Quetiapine misuse often begins with a desire for control, calm, or escape.
-
Self-medicating anxiety: People may take extra measures when stress spikes.
-
Using sedation as emotional relief: The “numbed” feeling becomes a coping mechanism.
-
Sleep fear or insomnia panic: Some individuals use higher doses when they can’t fall asleep quickly.
-
Trauma-related distress: Emotional overwhelm pushes people toward rapid-acting sedation.
-
Belief that “more will calm me faster”: Leads to dose stacking or repeated nightly misuse.
Environmental & Social Factors
Real-world circumstances strongly influence how quetiapine gets misused:
-
Easy access through prescriptions: Makes it simple to take more than prescribed.
-
Borrowing from friends or family: Common among individuals seeking sleep medication.
-
Chronic life stress (work, finances, relationships): Sedation becomes a quick escape.
-
Limited access to mental health care: People use quetiapine instead of therapy.
-
Unclear dosing instructions: Users increase doses when they don’t feel immediate calming.
-
Social environments with high emotional pressure: Encourage reliance on sedatives.
-
Lack of support systems: Isolation fuels nighttime or emergency misuse.
From Medical Use to Misuse (Progression)
The progression with quetiapine is behavioral and emotional, not driven by a classic addiction cycle.
-
Quetiapine is started for sleep, anxiety, or mood stabilization.
-
Users notice strong sedation and emotional quieting.
-
Stressful days lead to “just one extra tablet” for calming.
-
Over time, they increase the dose to achieve the same sleep or numbing effect.
-
Missing a dose causes rebound anxiety, restlessness, or insomnia.
-
Individuals start using it routinely to cope with stress, not just symptoms.
-
This forms a misuse loop: stress → quetiapine → temporary relief → more stress → higher dosing.
The cycle is driven by emotional dependence — not the traditional reward-driven dependence seen in addictive substances.
Who Is Most At Risk Of Developing Misuse Patterns?
-
People with co-occurring substance use disorders may use quetiapine to self-medicate or to multi-substance the effects.
-
Individuals prescribed quetiapine off-label for insomnia or anxiety — especially if follow-up is poor.
-
Younger adults and incarcerated populations, where diversion reports are more common.
-
People with poor sleep hygiene or untreated anxiety, who view medication as the primary sleep solution.
-
Those with multiple prescribers or inconsistent medication reconciliation increase the chance of duplication. [3]
Side Effects Of Quetiapine
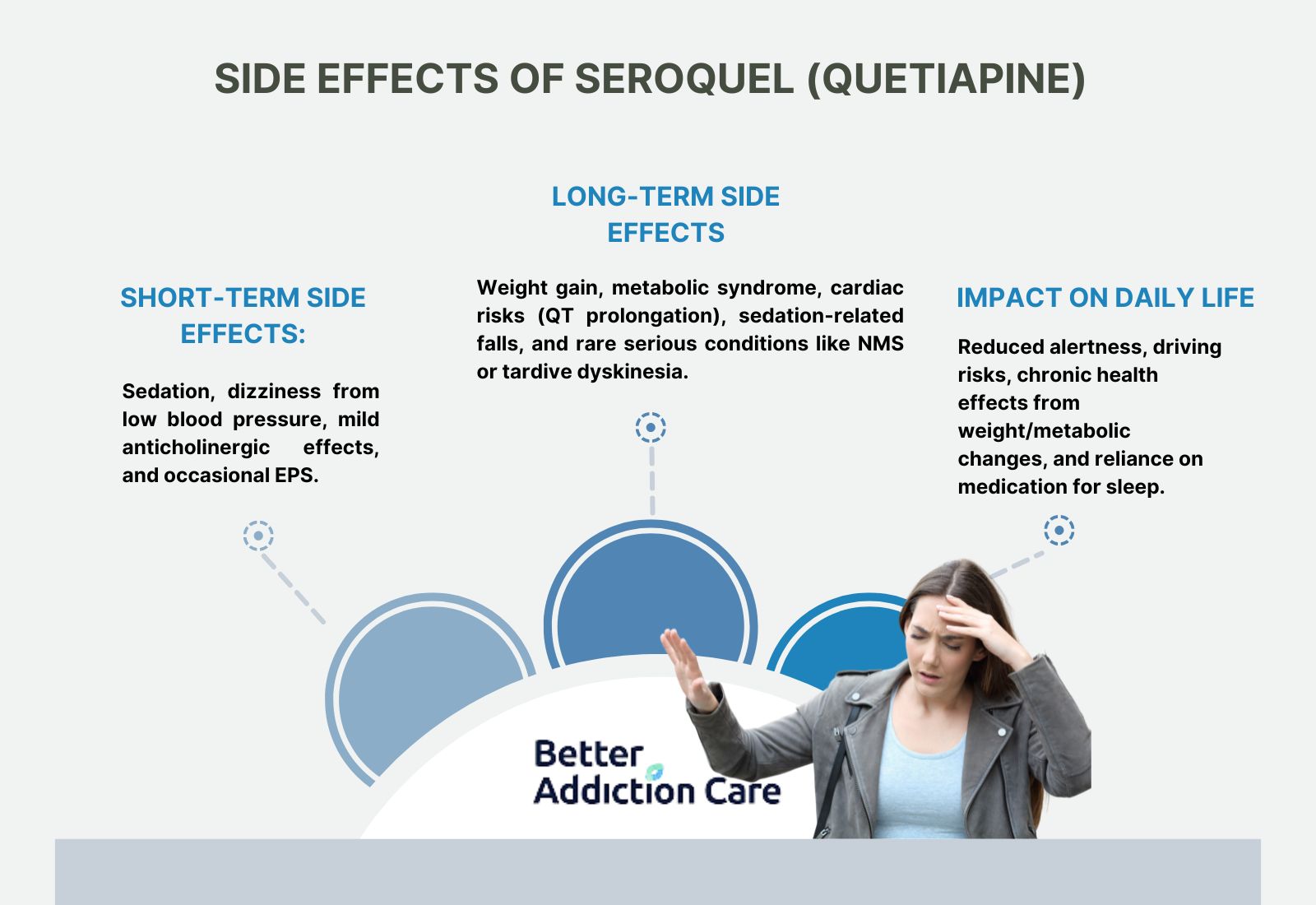
Short-Term Side Effects
-
Sedation and somnolence — very common, often dose-related
-
Orthostatic hypotension — dizziness on standing, especially at treatment initiation or with rapid dose increases.
-
Anticholinergic effects — dry mouth, constipation, although milder than older antipsychotics.
-
Extrapyramidal symptoms (EPS) — generally less common than with first-generation antipsychotics but possible, particularly at higher doses.
Long-Term Side Effects (Expanded)
-
Weight gain, metabolic syndrome, hyperglycemia, and dyslipidemia — clinically important risks that require monitoring. Long-term quetiapine treatment is associated with greater weight and metabolic effects than placebo in many trials.
-
Cardiac effects — QT prolongation is possible; baseline and periodic cardiac assessment may be indicated for at-risk patients.
-
Sedation-related morbidity — increased falls in older adults, daytime impairment in functioning.
-
Rare but serious: neuroleptic malignant syndrome (NMS), severe neutropenia, and tardive dyskinesia with long use (the latter is more associated with dopamine-blocking agents generally).
Impact On Daily Life
-
Reduced alertness and driving risks, especially if used for sleep and then dosed during the day.
-
Weight gain and metabolic effects can lead to chronic health conditions that affect function and longevity.
-
Sleep that is medication-dependent can undermine the development of behavioral sleep strategies.
Treatment Considerations When Misuse Or Problematic Patterns Appear
Because quetiapine misuse differs from classical substance addictions, treatment focuses on safe medication management, addressing underlying sleep/anxiety issues, and treating co-occurring substance use disorders.
Detox / Withdrawal Management
Quetiapine withdrawal does not resemble opioid or benzodiazepine withdrawal, but it can still be uncomfortable. Symptoms may include rebound insomnia, irritability, restlessness, mood swings, or heightened anxiety.
Clinicians decide whether a person needs outpatient support or a short inpatient stay based on their mental health stability. A sudden stop, or “cold turkey,” can worsen sleep disruption and emotional instability.
A supervised plan reduces discomfort and prevents relapse into misuse.
Supports:
-
Structured tapering: Gradually lowering the dose to avoid rebound symptoms.
-
Adjunct medications: Short-term use of non-addictive agents to manage sleep or anxiety.
-
Monitoring: Regular check-ins to assess mood, sleep quality, and risk of depressive relapse.
-
Stabilization planning: Identifying triggers that may worsen withdrawal symptoms.
Medication-Assisted Strategies (Not Traditional MAT)
Since quetiapine is not an opioid, traditional MAT is not used.
However, clinicians may still use supportive medications to manage underlying symptoms that contributed to misuse.
This helps individuals regain emotional balance while learning healthier coping methods.
Examples:
-
Non-addictive sleep aids: Help restore natural sleep cycles once sedative misuse stops.
-
SSRIs or SNRIs: Treat anxiety, depression, or trauma symptoms that may have led to overuse.
-
Mood stabilizers: Support individuals with bipolar disorder or mood dysregulation.
-
Beta-blockers: Reduce physical anxiety symptoms like rapid heart rate.
-
Short-term antihistamines: Provide temporary sleep support without addictive potential.
Levels of Care
Inpatient / Residential Treatment (30–90 Days)
-
Suitable for individuals with severe misuse, unstable mental health, or unsafe home environments.
-
Provides 24/7 supervision, structured routines, and medication management.
-
Daily therapy helps address emotional triggers, trauma, sleep disturbance, and co-occurring disorders.
-
The controlled setting removes access to misused medications and allows full focus on recovery.
Intensive Outpatient Program (IOP)
-
Ideal for people who need structured support but can still live at home.
-
Sessions occur several times a week and include group therapy, individual counseling, and psychiatric check-ins.
-
IOP helps individuals rebuild routines while learning coping skills for sleep, stress, and emotional regulation.
-
It provides accountability without full-time residential care.
Standard Outpatient Care
-
Weekly or biweekly therapy paired with medication management.
-
Great for long-term support after completing inpatient or IOP.
-
Helps individuals stay on track, adjust medications safely, and continue learning healthier habits.
Therapies
Behavioral therapies are essential for breaking emotional reliance on quetiapine.
CBT (Cognitive Behavioral Therapy):
-
Helps individuals understand the thoughts and fears that push them toward misuse.
-
Teaches strategies to manage nighttime anxiety, racing thoughts, and stress without medication.
-
Builds new habits that reduce emotional triggers.
Motivational Interviewing (MI):
-
Strengthens internal motivation for change.
-
Helps clients explore ambivalence, understand why misuse began, and build confidence in recovery.
Family Therapy:
-
Improves communication within the household.
-
Reduces conflict, stress, or misunderstanding that may have contributed to misuse.
-
Helps family members support healthy routines and medication boundaries.
Therapy focuses on coping skills, emotional stability, relapse prevention, and reducing dependence on sedation for comfort.
Peer Support & Recovery Capital
Peer groups create community and reduce the isolation that often fuels misuse. Individuals can share experiences, learn from others, and build accountability.
Recovery capital strengthens all areas of life — relationships, employment, stability, coping resources, and support networks.
Examples include:
-
NA or similar alternatives
-
SMART Recovery
-
Peer-led mental health support groups
-
Community wellness resources
These supports offer belonging and structure, which help reinforce long-term change.
Holistic Supports (Adjunct Care)
Holistic care strengthens emotional resilience without relying on sedating medications.
-
Mindfulness and meditation: Reduce stress and calm the nervous system.
-
Exercise routines: Improve sleep quality and balance mood naturally.
-
Sleep hygiene: Builds healthier bedtime habits to prevent nighttime anxiety.
-
Balanced nutrition: Supports steady energy and emotional stability.
-
Breathing techniques: Help during moments of panic or overwhelming stress.
-
Routine building: Reduces chaos and creates predictability, which lowers anxiety.
Stabilization & Immediate Safety
-
Assess for acute toxicity or dangerous combinations (e.g., heavy alcohol or opioid co-ingestion). Emergency management focuses on airway, breathing, circulation, and supportive care.
-
Stop hazardous combinations and ensure the person is in a setting where sedation and fall risk are minimized.
Tapering And Discontinuation Management
-
Slow, clinician-guided tapering is recommended to reduce discontinuation symptoms and rebound insomnia or anxiety. There is no universal taper schedule — individualization based on dose and duration is necessary. Systematic reviews show discontinuation symptoms are real and sometimes prolonged, so proactive planning matters.
-
Switching strategies: when quetiapine is discontinued for side effects, prescribers may switch to an alternative antipsychotic or a non-pharmacologic sleep strategy, depending on the indication.
Withdrawal / Discontinuation Timeline — What To Expect?
Quetiapine does not produce classic addictive cravings via reward circuitry, but abrupt discontinuation after weeks to months of treatment can cause a cluster of discontinuation symptoms.
Typical pattern seen:
-
Within 1–4 days: insomnia, anxiety, agitation, nausea, sweating, tremor, and autonomic symptoms can begin.
-
First 1–2 weeks: rebound of original psychiatric symptoms (e.g., return of psychosis or mood instability) or new symptoms such as increased anxiety or rebound insomnia.
-
Up to several weeks: most discontinuation symptoms subside within 1–3 weeks if managed appropriately, though some patients report longer, persistent symptoms. Rarely, movement disorders (withdrawal dyskinesia) have been reported. [6]
When To Seek Immediate Help?

Seek urgent care or emergency services if any of the following occur:
-
Severe difficulty breathing, swelling of the face or throat, or signs of anaphylaxis (rare but life-threatening).
-
Loss of consciousness, severe hypotension, or collapse (possible in overdose or in dangerous drug combinations).
-
Sudden, severe chest pain or neurologic changes (confusion, fainting, seizures) — evaluate for cardiac or neurologic emergencies.
-
Severe agitation, suicidal ideation, or psychotic symptoms — urgent psychiatric evaluation is needed.
Dosing & Safety / Overdose Risks
Typical Therapeutic Ranges & Formulations
-
Prescribed within defined therapeutic windows based on the condition and symptom severity.
-
Lower doses are often used for sleep or anxiety; moderate to higher doses for mood stabilization or psychosis.
-
Available in immediate-release (IR) and extended-release (XR) formulations.
-
Dose adjustments are done gradually to avoid excessive sedation, low blood pressure, or next-day impairment.
-
Clinicians individualize dosing based on age, medical comorbidities, response, and medication interactions.
High-Risk Combinations
-
Alcohol significantly increases sedation and impairs coordination, raising accidental injury and overdose risk.
-
Benzodiazepines, opioids, and other sedatives amplify central nervous system depression when taken with quetiapine.
-
These combinations can rapidly shift quetiapine from safe to dangerous, even at therapeutic doses.
-
Extra caution is required in individuals with respiratory issues or low medication tolerance.
Overdose Mechanism
-
Overdose can lead to extreme drowsiness, confusion, low blood pressure, slowed breathing, and loss of consciousness.
-
The most serious danger is respiratory depression, especially during polysubstance use.
-
If opioids are involved, naloxone can quickly reverse breathing problems and save the person’s life.
-
Medical evaluation is essential because quetiapine toxicity can worsen over time, even if symptoms start mild.
Safe Use Practices
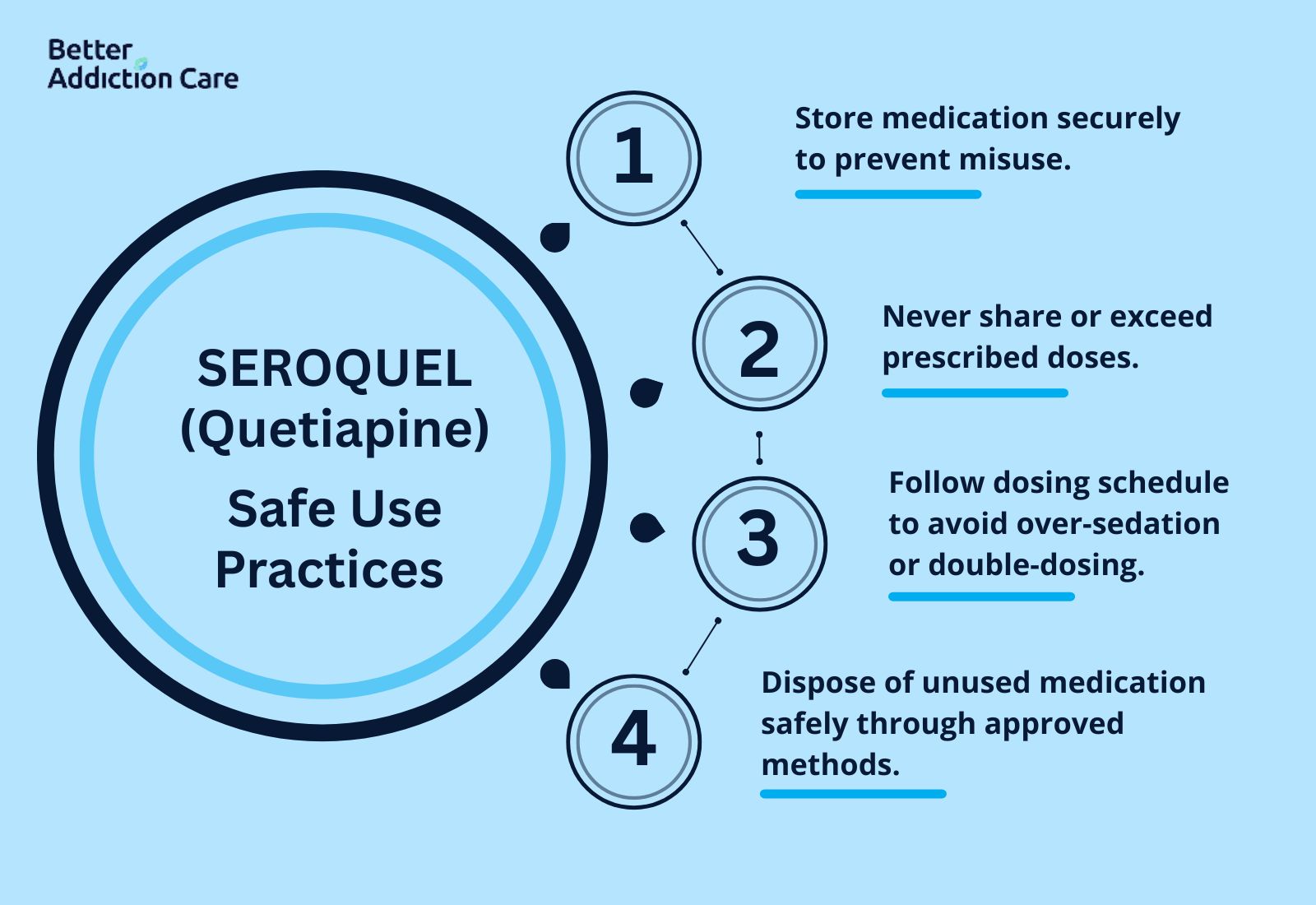
-
Store medication securely to prevent access by children, teens, or individuals with a substance misuse risk.
-
Do not share tablets or take more than prescribed under any circumstances.
-
Follow the prescribed schedule closely to prevent over-sedation or accidental double-dosing.
-
Dispose of unused or discontinued medication through pharmacy take-back programs or approved disposal methods.
Conclusion
Quetiapine is an effective medication for serious mental health conditions when used as prescribed.
While it is not highly addictive, misuse, dose escalation, and withdrawal symptoms can occur. Safe use means taking it only when needed, avoiding routine use for sleep, monitoring health, and tapering gradually under medical supervision.
If you or a loved one is using quetiapine irregularly, taking extra doses, or is worried about stopping:
-
Talk to your doctor openly about how you use the medication and any other substances.
-
Do not stop suddenly; follow a safe taper plan.
-
Use non-drug strategies for sleep and anxiety, like CBT-I, sleep hygiene, or therapy.
-
Get a medical evaluation for concerning side effects (excessive sedation, falls, changes in mood, signs of metabolic syndrome).
FAQs
No, Quetiapine does not cause the “high” that addictive drugs do and is not a controlled substance. However, it can still be misused, taken in higher doses than prescribed, shared with others, or cause withdrawal symptoms if stopped suddenly. So, saying it is “not addictive” does not mean it is completely risk-free.
The most serious dangers happen when quetiapine is combined with alcohol, opioids, or other sedatives. Misuse can lead to extreme drowsiness, slowed breathing, low blood pressure, or life-threatening complications. Always take quetiapine exactly as prescribed and store it safely to prevent accidental overdose.
Relapse is common and does not mean failure. It usually occurs when stress, sleep problems, or emotional triggers return. Relapse indicates that the treatment plan may need adjustment and additional support. With proper guidance, people can regain healthy routines and avoid further misuse.
No. Stopping quetiapine suddenly can cause insomnia, anxiety, agitation, and rebound symptoms. The safest approach is a gradual taper under medical supervision, which reduces withdrawal effects and supports recovery.
Families can play a key role by learning about quetiapine withdrawal and misuse, offering non-judgmental support, encouraging therapy, and helping maintain healthy daily routines. Observing warning signs in a supportive way can prevent relapse and improve recovery outcomes.
Quetiapine withdrawal is rarely life-threatening, unlike opioid or alcohol withdrawal. Risks increase if doses are stopped abruptly or combined with other sedatives. Supervised tapering is the safest method to manage withdrawal and ensure long-term safety.
Resources
Related Articles
Treatment Centers in Texas










