Seroquel Withdrawal: Symptoms, Timeline, and Care Tips
When Seroquel is stopped abruptly, the brain does not have enough time to readjust its neurotransmitter activity. The sudden gap between medication removal and neurochemical stability can lead to symptoms like anxiety, insomnia, agitation, and physical discomfort.

Key Takeaways
-
Is withdrawal real? → Yes. Seroquel withdrawal can happen, but it’s temporary and becomes much easier to handle with the right support. Most people notice symptoms easing week by week as their system recalibrates.
-
How should I stop safely? → A slow, medically supervised taper is the safest way to let your brain adjust without sudden shocks. This approach lowers the risk of rebound symptoms and keeps you more comfortable throughout the process.
-
What helps recovery? → Consistent routines, healthy habits, therapy, and strong support systems help your body and mind stabilize as you recover.
What Seroquel Is and How It Works?
Seroquel (quetiapine) is an atypical antipsychotic used to treat conditions such as bipolar disorder, schizophrenia, and certain anxiety or sleep-related issues. It works by influencing key neurotransmitters—primarily dopamine and serotonin—that regulate mood, thought patterns, and sleep. [1]
Over time, the brain becomes accustomed to this external support and adjusts its own production and receptor sensitivity. This is not harmful in itself, but it does mean the brain has to gradually relearn balance when the medication is reduced.
Understanding this biological shift helps people recognize that withdrawal symptoms are not signs of weakness, but simply signals that the body is recalibrating.
Why Stopping Suddenly Can Trigger Withdrawal?
When Seroquel is stopped abruptly, the brain does not have enough time to readjust its neurotransmitter activity. The sudden gap between medication removal and neurochemical stability can lead to symptoms like anxiety, insomnia, agitation, and physical discomfort.
These reactions do not mean the medication was harmful—they simply reflect how deeply the central nervous system relies on stability. Abrupt withdrawal is like slamming the brakes on a moving car: the body feels the jolt.
Tapering slowly gives the brain time to gently restore its natural balance, reducing distress and helping people stay emotionally grounded through the transition.
Withdrawal vs. Relapse — Understanding the Difference
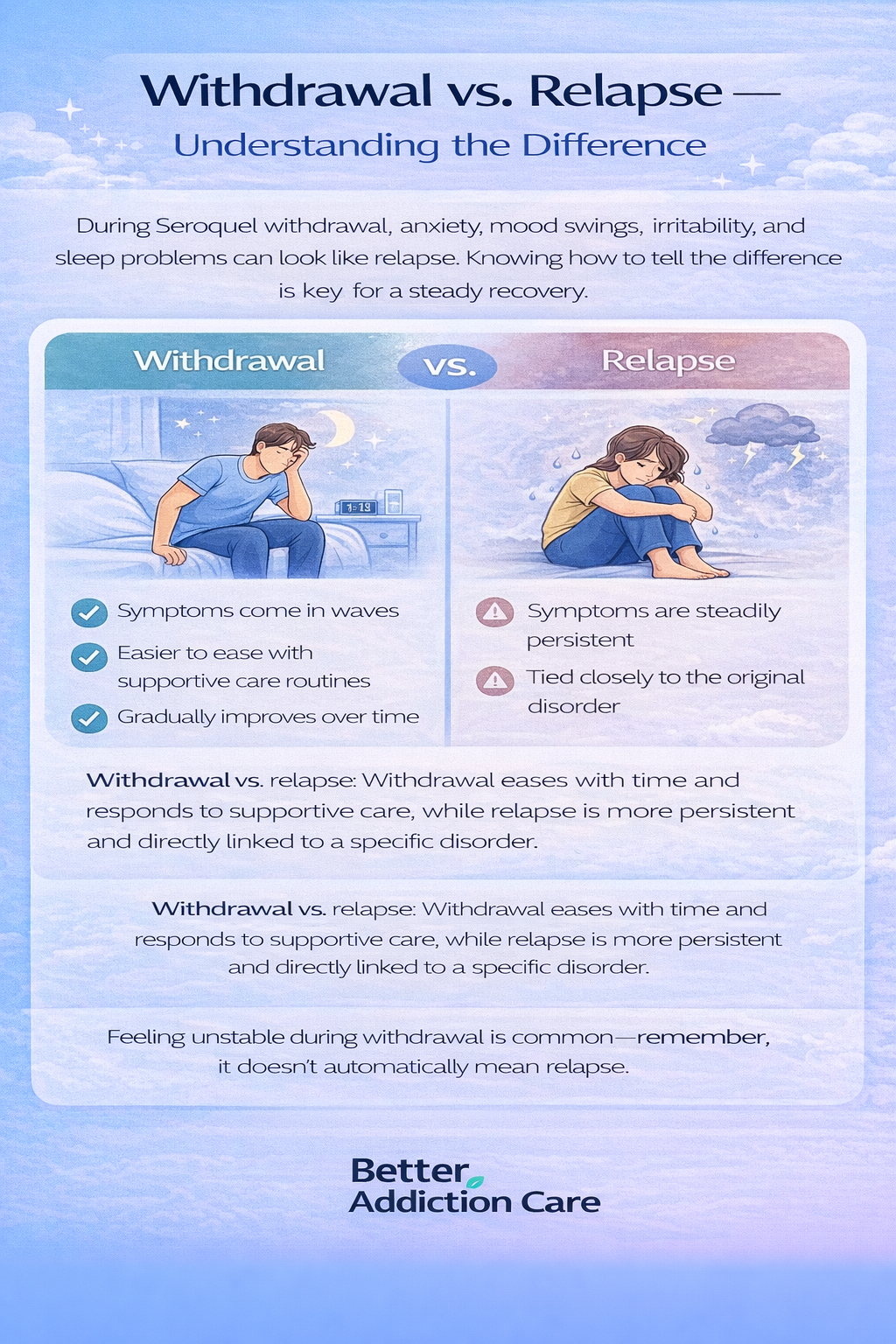
One of the most confusing experiences during Seroquel withdrawal is differentiating between withdrawal symptoms and a true return of the original condition. Withdrawal often causes anxiety, mood swings, irritability, and sleep problems that can look very similar to relapse.
The key difference is timing and pattern: withdrawal tends to come in waves, ease over weeks, and respond to supportive care routines, while relapse is more persistent and tied directly to the underlying disorder.
A clinician can help distinguish the two, but emotionally, it’s important to remember that feeling unstable during withdrawal does not automatically mean relapse. It often means the brain is healing.
Withdrawal Is Not Addiction
Many people fear that experiencing withdrawal might mean they were “addicted” to Seroquel. This fear creates shame and anxiety that only worsens symptoms. But medically, Seroquel is not considered an addictive drug. There are no cravings, compulsive use, or drug-seeking behaviors.
What people experience is physical dependence: the body adapts to a medication over time and needs a gradual reduction to adjust. Dependency is biological; addiction is behavioral. Withdrawal is simply your body finding its equilibrium again—nothing more, nothing less.
What Are the Common Symptoms of Seroquel Withdrawal?
Physical Symptoms
Physical withdrawal symptoms often show up first, and they can feel surprisingly intense for such a commonly prescribed medication. People may experience dizziness, nausea, headaches, sweating, fatigue, body aches, or flu-like sensations. Others describe a feeling of inner restlessness or a racing heartbeat. [2]
While uncomfortable, these symptoms are almost always time-limited and improve significantly during the tapering process. It helps to remember that these reactions reflect healing, not harm. The body is working hard to re-stabilize, and although the process is uncomfortable, it is also temporary.
Sleep Disturbances
Because Seroquel has sedative properties, sleep disruption is one of the most common withdrawal challenges. People may struggle with insomnia, fragmented sleep, intense or vivid dreams, night sweats, or early-morning awakening. These symptoms often peak in the first one to two weeks and gradually improve as the brain resets its natural sleep cycle.
Sleep may feel unpredictable at first, but with gentle routines—consistent bedtimes, reduced screens, and calming rituals—the body slowly regains its rhythm. It’s important to remind individuals that the inability to sleep is a symptom, not a failure, and it will not last forever.
Emotional and Mental Health Symptoms
Emotional turbulence can be one of the most difficult parts of Seroquel withdrawal. Anxiety may spike unexpectedly, mood swings can feel dramatic, and irritability or sadness may rise without warning. These changes often reflect the brain’s temporary difficulty regulating serotonin and dopamine while adjusting to life without the medication’s stabilizing effects.
Families and individuals should understand that emotional swings during this period do not define them and are not a return of their original disorder. With support, coping tools, and a structured taper, most people experience steady emotional improvement.
Sensory or Neurological Symptoms
Some individuals experience “brain zaps,” sensitivity to light or sound, tremors, or a sense of inner agitation. While these symptoms can be scary, they are usually short-lived and tend to improve significantly once the tapering schedule slows down.
They are signs of the nervous system reorganizing itself—an uncomfortable but temporary part of recovery. Gentle reassurance, grounding exercises, and staying hydrated can help ease these sensations until they pass.
What Is the Typical Seroquel Withdrawal Timeline?

Days 1–3: Early Withdrawal
During the first few days, people may notice mild nausea, headaches, dizziness, or irritability. Sleep may begin to shift, and the body may feel slightly off-balance. This stage is uncomfortable but usually manageable, especially with a slow taper. [3]
Weeks 1–2: Peak Discomfort
This is often the most intense phase. Anxiety may feel stronger, sleep may be severely disrupted, and physical symptoms like sweating, agitation, or mood changes may intensify. It’s important to remember that this peak is a normal part of healing, not a sign that something is wrong. Support systems are essential here—patients should not navigate this stage alone.
Weeks 3–4: Improvement Phase
By the third and fourth weeks, the body typically begins to settle. Sleep becomes more predictable, emotional swings ease, and energy starts to return. People often report moments of clarity or mental sharpness that feel encouraging. This stage is a sign that the brain is adapting successfully.
After 1 Month: Adjustment Phase
Some individuals may still notice occasional mood dips, fatigue, or sleep variation, but symptoms usually become far less intense. The focus shifts from symptom management to rebuilding steady routines and long-term wellness. This is where lifestyle habits truly begin to support stability.
Why Timelines Vary?
Everyone’s withdrawal timeline is unique. Factors such as dosage, length of use, taper speed, metabolism, and co-occurring mental health conditions all influence how long symptoms last.
Compassion, patience, and individualized guidance are essential during this journey.
Why Should Seroquel Be Tapered Slowly?
Risks of Stopping Cold Turkey
Stopping Seroquel suddenly can trigger a strong rebound response from the brain. Many people experience severe insomnia that appears almost overnight, leaving them unable to rest or function normally.
Emotional stability can also crash quickly, leading to irritability, sudden waves of sadness, restlessness, or even brief episodes of panic.
You may also feel mentally foggy or disoriented, which can make everyday tasks harder. These reactions often feel alarming, and many people mistake them for a return of their original condition. In reality, these symptoms usually reflect withdrawal distress — the brain struggling to adjust after losing the medication too fast.
Benefits of Slow Tapering
A slow, supervised taper gives the brain time to rebalance gradually rather than being shocked all at once. Reducing the dose in small steps helps minimize discomfort and lowers the risk of intense withdrawal symptoms.
It also creates a more stable emotional environment, making it easier for you and your clinician to track what’s truly happening. [4]
During a slow taper, people often feel more in control because changes are predictable and manageable. This approach also helps differentiate between temporary withdrawal sensations and genuine relapse, which is crucial for long-term success. A gentle taper supports the nervous system so it can adjust safely and steadily.
“Go Slow to Go Steady” Principle
Tapering Seroquel is not a race. It should be personalized to your needs, your history, and your body’s reactions—not based on a fixed schedule. Some people may taper over several months, while others need a longer, more gradual process to stay stable.
The goal is steady progress, not speed. Working closely with a clinician ensures each adjustment is safe and tolerable. When tapering is done slowly and thoughtfully, people typically experience fewer setbacks and feel more confident in their ability to transition off the medication.
How Healthcare Providers Help You Safely Manage Seroquel Withdrawal Symptoms?
Monitoring Symptoms and Adjusting the Taper
Healthcare providers help make the withdrawal process safer and more predictable. They track your symptoms carefully, paying attention to changes in sleep, mood, and physical comfort.
This isn’t guesswork — withdrawal affects the nervous system, and small dose shifts can have real effects.
When symptoms rise too quickly, your provider can slow the taper, use smaller dose reductions, or pause for stabilization. This approach protects your well-being and acknowledges a simple truth: every brain adapts at its own pace, and forcing the process often leads to unnecessary suffering.
Distinguishing Withdrawal From Relapse
It’s common to fear that every bad day means relapse, but science and clinical experience show that withdrawal and relapse look different. Withdrawal often causes temporary irritability, restlessness, and sleep disruption because the brain is recalibrating.
A provider helps interpret these patterns with clarity and calmness. They can explain what’s expected, what’s concerning, and what’s simply part of the adjustment period. This guidance provides emotional grounding and reduces the panic that often makes withdrawal feel worse than it truly is.
Offering Reassurance and Short-Term Support
Withdrawal can feel overwhelming, and it’s normal to need reassurance. A good clinician offers more than instructions — they offer presence. They validate what you’re experiencing and remind you that these symptoms, while uncomfortable, are usually temporary.
If certain symptoms become too difficult, short-term medications may be used to ease things. These aren’t long-term solutions but tools to help your body move through a stressful period more smoothly. The goal is comfort, not dependency.
Tracking Overall Mental Health to Prevent Setbacks
Tapering is not just about reducing a number on a pill bottle — it’s about protecting your overall mental health.[4] Providers monitor how you’re functioning day to day: your mood stability, ability to cope with stress, concentration, and emotional resilience.
By keeping a close eye on these factors, they can intervene early if something starts to slip. This proactive support reduces the risk of setbacks and helps you feel less alone during the transition.
What Coping Strategies Help During Withdrawal?
1. Improving Sleep
A predictable sleep routine does wonders during withdrawal. This can include maintaining a consistent bedtime, using low light in the evenings, avoiding caffeine late in the day, and using grounding techniques like deep breathing or warm baths. These habits help retrain the brain’s natural circadian rhythm and reduce nighttime tension.
2. Supportive Eating and Hydration
Balanced meals rich in protein, whole grains, and vegetables help stabilize energy and mood. Hydration supports the brain and reduces headaches and fatigue. Eating smaller, regular meals can also help with nausea and prevent blood sugar swings that worsen anxiety.
3. Gentle Movement and Exercise
Light physical activity—walking, stretching, yoga—helps regulate mood, reduce stress, and improve sleep quality. [5] Intense workouts are not recommended early in withdrawal, as they may increase agitation. Slow, steady movement is more effective for nervous-system healing.
4. Reducing Stress and Anxiety
Mindfulness practices, journaling, guided breathing, grounding exercises, and therapy techniques can all help reduce the emotional intensity of withdrawal. These tools give people a sense of control when emotions feel unpredictable.
5. Staying Connected and Supported
Having someone to talk to—whether a family member, friend, or therapist—makes a significant difference. Support reduces isolation, helps people maintain perspective, and allows for shared responsibility during challenging moments. Withdrawal should not be faced alone.
6. The Power of Routine
Daily structure reduces anxiety and helps the brain rebuild stability. Predictable routines around meals, sleep, work, and relaxation send steady signals to the nervous system that things are safe and manageable.
When Should I Seek Medical Help During Withdrawal?
Seek medical help immediately if withdrawal symptoms include severe agitation, suicidal thoughts, hallucinations, dangerous changes in heart rate, or extreme insomnia lasting multiple nights.
These symptoms require immediate evaluation and should not be ignored.
When to Call the Prescribing Doctor
If symptoms persist beyond the expected timeline, if the emotional intensity becomes unmanageable, or if there is uncertainty about relapse, contacting the prescribing provider is important. Adjusting the taper or adding supportive care may be necessary.
What Comes After Withdrawal?

Rebuilding Natural Rhythms
After the tapering process, the body begins to rediscover its own pace—sleep cycles normalize, appetite evens out, and emotional regulation becomes more predictable. This rebalancing may take time, but it is one of the most promising stages of recovery.
Ongoing Mental Health Support
Therapy, lifestyle changes, and consistent check-ins with mental health providers are essential after withdrawal. These tools build resilience and help prevent relapse by supporting long-term emotional stability.
Recovery as an Ongoing Journey
Withdrawal is just one chapter, not the entire story. Recovery continues beyond the symptoms. People often find new strengths, healthier routines, and greater self-awareness. Healing is not linear, but it is absolutely possible with patience and support.
Conclusion
Seroquel withdrawal can feel overwhelming, but it is a temporary and manageable process that improves with the right support and a gentle, medically guided approach. With patience, steady habits, and a strong support system, most people regain stability and develop healthier rhythms that support their long-term mental well-being.
Recovery is not about rushing—it is about healing at a pace the brain can tolerate. With the right guidance and compassion, the journey becomes not just survivable but transformative.
FAQs
No. Stopping suddenly can overwhelm your nervous system and trigger severe insomnia, anxiety, and emotional instability. These reactions often feel like relapse but are usually withdrawal. A slow, supervised taper is the safest option.
Most people see major symptoms improve within 2–4 weeks. However, mild sleep or mood changes may linger a bit longer. The timeline varies based on your dose, duration of use, and how gradually you taper.
Withdrawal can mimic relapse with irritability, restlessness, or mood swings, but these symptoms often fade as the brain adjusts. A doctor can help you tell the difference and guide you through what’s normal versus concerning.
Steady sleep habits, hydration, light exercise, and mindfulness practices can ease discomfort. Following a structured taper and staying connected with supportive people also helps your body adjust more calmly.
Loved ones can help by being patient, offering reassurance, and helping maintain routines. Staying present during emotional or sleep disruptions gives the person stability and reduces feelings of isolation.
If symptoms become too intense—such as severe insomnia, panic, or confusion—contact your doctor right away. You may need a slower taper or short-term support to stabilize. Early help prevents worsening withdrawal.









