Seroquel Overdose Symptoms, Risks, and Emergency Response
Seroquel (quetiapine) is a prescription medication commonly used to treat conditions such as bipolar disorder, schizophrenia, and major depressive disorder. A Seroquel overdose can affect breathing, heart rhythm, blood pressure, and consciousness, and symptoms may worsen faster than families expect. Quick action can save a life.

Key Takeaways
-
Seroquel overdose can cause severe symptoms rapidly
-
Breathing problems and unconsciousness are medical emergencies
-
Immediate emergency response is essential
-
Most people recover fully with prompt treatment
-
Ongoing medical supervision significantly reduces overdose risk
While it can be effective when taken as prescribed, overdose can occur—sometimes accidentally—due to dose confusion, mixing substances, or underlying medical vulnerabilities.
A Seroquel overdose can affect breathing, heart rhythm, blood pressure, and consciousness, and symptoms may worsen faster than families expect. Quick action can save a life.
This article explains how Seroquel overdose occurs, what warning signs to look out for, and what to do in an emergency. This information is educational only and should not be considered medical advice. Suspected overdose requires immediate emergency care.
What Is Seroquel & Why Is Overdose Possible?
Seroquel is the brand name for quetiapine, an atypical antipsychotic medication. It works by altering how certain chemical messengers—primarily dopamine and serotonin—function in the brain. These neurotransmitters play a major role in mood regulation, perception, sleep, and emotional stability.
At therapeutic doses, Seroquel helps stabilize brain signaling. In excessive amounts, however, the medication can over-suppress the central nervous system, meaning the brain areas responsible for alertness, breathing, heart rate, and blood pressure become overwhelmed.
Overdose is possible because:
-
Dose sensitivity varies widely between individuals
-
Extended-release (XR) formulations release medication slowly, which can delay symptom onset
-
The drug affects multiple body systems, not just mood
In simple terms, overdose happens when the body receives more quetiapine than it can safely process, leading to dangerous shutdowns in vital systems—especially when combined with alcohol or other depressants.
Early Signs of a Seroquel Overdose
These symptoms often appear first and are frequently mistaken for deep sedation, extreme fatigue, or “sleeping off” medication effects. This is especially dangerous because early overdose signs can quietly worsen without obvious warning.
-
Severe drowsiness or inability to stay awake
Your loved one may struggle to keep their eyes open, fall asleep mid-conversation, or be difficult to wake. This goes beyond normal medication-related sleepiness and signals excessive central nervous system suppression. -
Confusion or disorientation
They may seem mentally “foggy,” give inappropriate answers, forget where they are, or appear disconnected from their surroundings. -
Difficulty speaking clearly or responding appropriately
Speech may become slow, slurred, or delayed, and responses may not match the questions being asked, indicating impaired brain signaling. -
Sudden drop in blood pressure, causing dizziness or faintness
Standing up may lead to lightheadedness, weakness, or collapse, as the body struggles to maintain normal circulation. -
Blurred vision or abnormal eye movements
Vision changes, difficulty focusing, or unusual eye motion can occur as the nervous system becomes overstressed. -
Agitation, restlessness, or unusual behavior changes
Instead of calm sedation, some individuals become restless, anxious, or behave in ways that feel out of character, which can be an early warning sign of toxicity.
Severe / Life-Threatening Overdose Symptoms
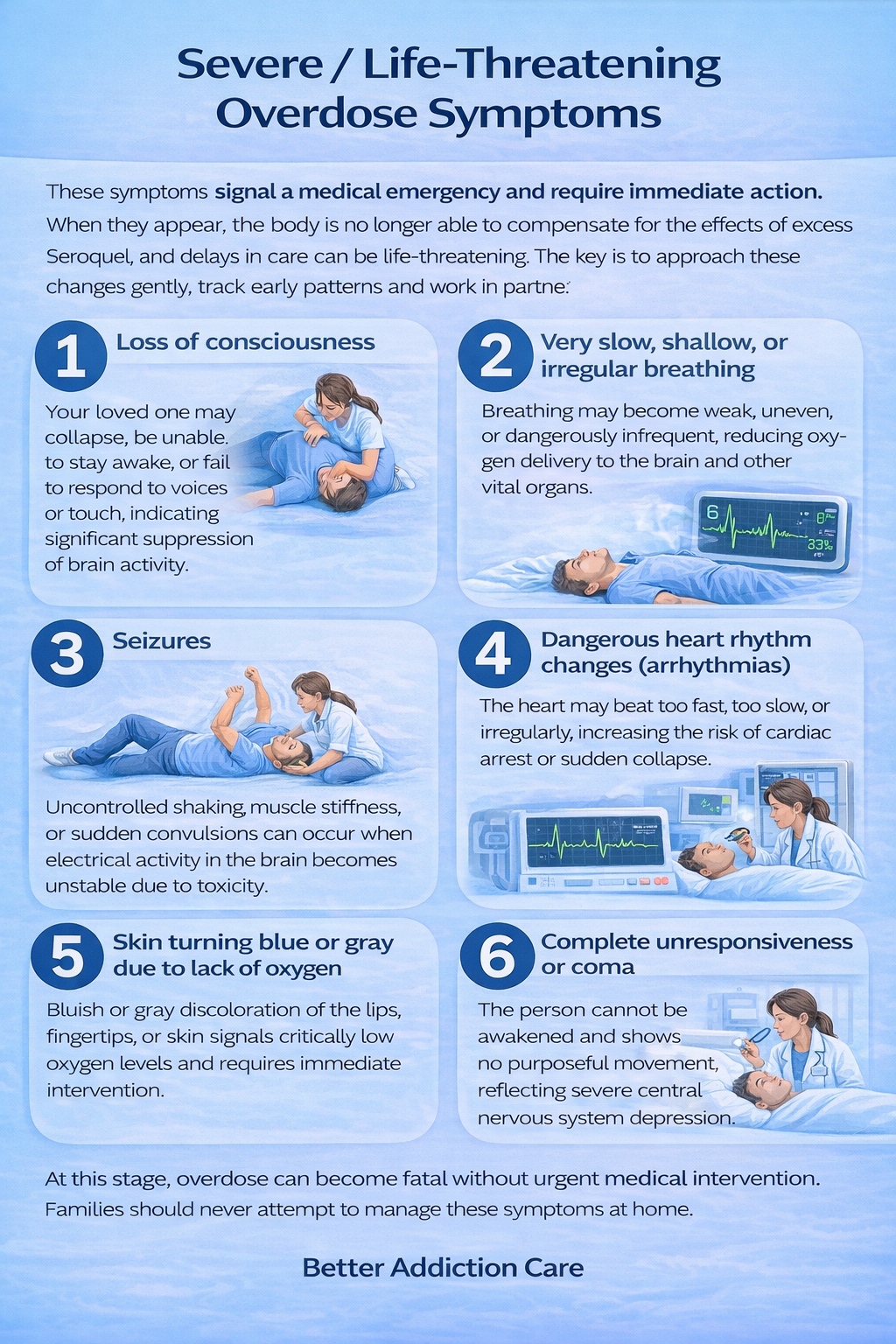
These symptoms signal a medical emergency and require immediate action. When they appear, the body is no longer able to compensate for the effects of excess Seroquel, and delays in care can be life-threatening.
-
Loss of consciousness
Your loved one may collapse, be unable to stay awake, or fail to respond to voices or touch, indicating significant suppression of brain activity. -
Very slow, shallow, or irregular breathing
Breathing may become weak, uneven, or dangerously infrequent, reducing oxygen delivery to the brain and other vital organs. -
Seizures
Uncontrolled shaking, muscle stiffness, or sudden convulsions can occur when electrical activity in the brain becomes unstable due to toxicity. -
Dangerous heart rhythm changes (arrhythmias)
The heart may beat too fast, too slow, or irregularly, increasing the risk of cardiac arrest or sudden collapse. -
Skin turning blue or gray due to lack of oxygen
Bluish or gray discoloration of the lips, fingertips, or skin signals critically low oxygen levels and requires immediate intervention. -
Complete unresponsiveness or coma
The person cannot be awakened and shows no purposeful movement, reflecting severe central nervous system depression.
At this stage, overdose can become fatal without urgent medical intervention. Families should never attempt to manage these symptoms at home.
What Causes a Seroquel Overdose?
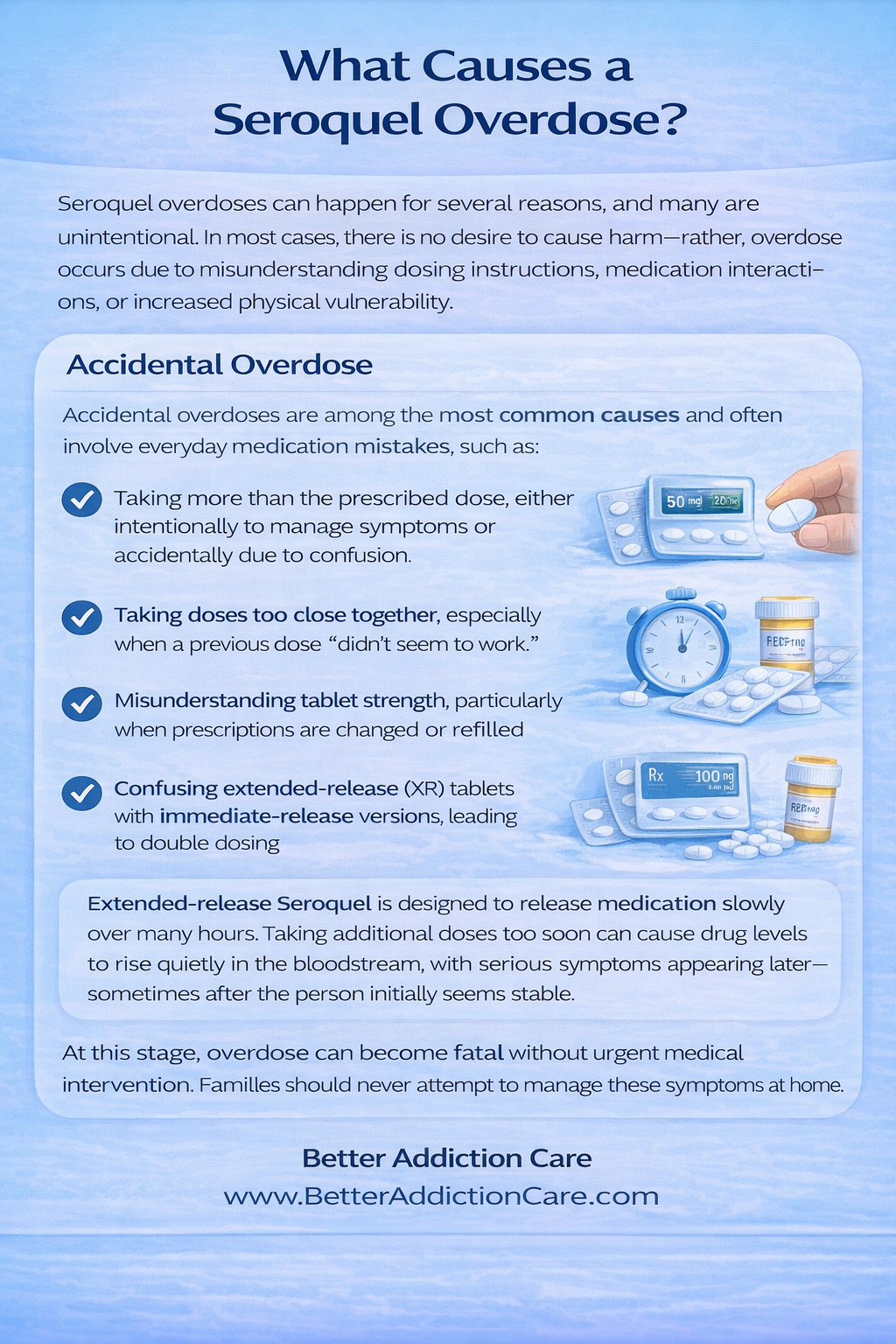
Seroquel overdoses can happen for several reasons, and many are unintentional. In most cases, there is no desire to cause harm—rather, overdose occurs due to misunderstanding dosing instructions, medication interactions, or increased physical vulnerability.
Accidental Overdose
Accidental overdoses are among the most common causes and often involve everyday medication mistakes, such as:
-
Taking more than the prescribed dose, either intentionally to manage symptoms or accidentally due to confusion
-
Taking doses too close together, especially when a previous dose “didn’t seem to work.”
-
Misunderstanding tablet strength, particularly when prescriptions are changed or refilled
-
Confusing extended-release (XR) tablets with immediate-release versions, leading to double dosing
Extended-release Seroquel is designed to release medication slowly over many hours. Taking additional doses too soon can cause drug levels to rise quietly in the bloodstream, with serious symptoms appearing later—sometimes after the person initially seems stable.
Mixing With Other Substances
Combining Seroquel with other substances significantly increases overdose risk, especially when those substances also slow brain and body functions. High-risk combinations include:
-
Alcohol
-
Opioids, such as oxycodone or fentanyl
-
Sleep medications
-
Benzodiazepines, including Xanax or Valium
All of these substances depress the central nervous system, which controls breathing, heart rate, and alertness.
When used together, their effects can stack rather than cancel out, dramatically increasing the risk of breathing suppression, coma, or fatal overdose. This synergistic depressant effect is one of the leading contributors to severe Seroquel overdose cases [1].
Underlying Health Conditions
Certain medical conditions make the body less able to process and eliminate Seroquel, increasing overdose risk even at standard doses:
-
Liver or kidney disease, which slows the breakdown and removal of the medication
-
Heart conditions, especially those affecting rhythm or blood pressure regulation
-
Respiratory disorders, such as sleep apnea or chronic obstructive pulmonary disease (COPD)
-
Age-related vulnerability, particularly in older adults with slower metabolism
In these individuals, quetiapine may remain in the body longer and accumulate, allowing toxic levels to develop more easily. This is why close medical monitoring and dose adjustments are especially important for higher-risk populations.
Short-Term Health Risks
A Seroquel overdose can trigger rapid, life-threatening complications that affect multiple vital systems at once. These risks can develop quickly and may worsen even if symptoms seem stable at first.
-
Breathing suppression, reducing oxygen to the brain
Seroquel can slow or weaken breathing, limiting oxygen delivery to the brain and other organs. Even short periods of reduced oxygen can cause serious neurological harm.
-
Heart rhythm irregularities, increasing cardiac arrest risk
Overdose can disrupt the heart’s electrical signaling, leading to dangerously fast, slow, or irregular heartbeats that raise the risk of sudden cardiac collapse.
-
Aspiration, where vomit enters the lungs
Excessive sedation or unconsciousness can impair the gag reflex, allowing vomit to enter the airway and lungs, which may cause choking, pneumonia, or respiratory failure.
-
Severe low blood pressure, leading to collapse or shock
A sudden drop in blood pressure can reduce blood flow to vital organs, causing dizziness, fainting, or life-threatening shock.
-
Acute stress on organs, especially the heart and brain
The combined effects of low oxygen, unstable blood pressure, and abnormal heart rhythms place intense strain on the body, increasing the risk of organ injury.
Long-Term Complications After an Overdose
While many people recover fully with timely treatment, severe overdoses can cause lasting effects—especially if oxygen deprivation occurred.
Early emergency care significantly reduces the likelihood of long-term complications [2].
What to Do If You Suspect a Seroquel Overdose?
Act immediately. Do not wait for symptoms to progress.
1. Call for emergency help
-
Dial 911 or your local emergency number right away
-
Clearly state that a Seroquel (quetiapine) overdose is suspected
2. Stay with your loved one
-
Do not leave them alone
-
Watch for changes in breathing, color, or responsiveness
-
If they are awake, keep them gently engaged
3. Protect their airway
-
If they vomit or seem drowsy, turn them onto their side
-
This helps prevent choking if consciousness decreases
4. Avoid unsafe actions
-
Do not give food, drinks, alcohol, or more medication
-
Do not try home remedies or wait for improvement
5. Prepare key information for responders
Have this ready if possible:
-
When Seroquel was taken
-
How much may have been taken
-
Whether alcohol or other drugs were involved
Quick, honest communication helps medical teams act faster and more effectively.
Hospital Treatment (High-Level Overview)
There is no specific antidote for a Seroquel (quetiapine) overdose. Medical care focuses on keeping vital systems functioning safely while the body gradually processes and clears the medication. Treatment is tailored to symptom severity and may change as the patient’s condition evolves.
Primary goals of hospital care
-
Maintain safe breathing and oxygen levels
-
Protect heart rhythm and blood pressure
-
Prevent complications such as seizures or aspiration
What do medical teams typically do?
-
Close, continuous monitoring: Heart rhythm, breathing rate, blood pressure, and oxygen levels are tracked around the clock to catch sudden changes early.
-
Circulatory support: IV fluids are commonly used to stabilize low blood pressure and support organ function.
-
Breathing assistance when needed: Supplemental oxygen is provided if breathing slows. In more severe cases, airway support may be required to ensure adequate oxygen delivery to the brain.
-
Targeted treatment for complications: Medications may be administered to control seizures, agitation, or abnormal heart rhythms if they occur.
-
Extended observation for delayed effects: Because symptoms—especially from extended-release Seroquel—can worsen hours later, patients remain under supervision until it is medically safe to discharge.
How long does monitoring last?
Most individuals are observed for 24–72 hours, depending on overdose severity, response to treatment, and the formulation involved [3].
Who Is at Higher Risk of Seroquel Overdose?
Certain groups face increased risk:
-
Children and older adults: Smaller body size, age-related changes in metabolism, and increased sensitivity to sedating effects raise overdose risk even at lower doses.
-
People taking multiple prescription medications: Drug interactions—especially with other sedatives, opioids, or blood pressure medications—can intensify respiratory depression and heart rhythm disturbances.
-
Individuals with heart or lung conditions: Pre-existing cardiovascular or respiratory disease increases the danger of low blood pressure, slowed breathing, or dangerous rhythm changes.
-
Those with a history of substance misuse: Higher tolerance, misuse patterns, or combining Seroquel with alcohol or other drugs significantly increases overdose risk.
-
People using Seroquel off-label for sleep without close monitoring: Dose escalation, inconsistent use, or lack of medical follow-up can lead to accidental overuse.
Understanding risk factors allows families and providers to implement preventive safeguards early.
Preventing Overdose
Prevention focuses on clarity, communication, and ongoing monitoring, especially when Seroquel is used long-term or alongside other medications.
-
Follow prescriptions exactly as written, including the dose, timing, and formulation.
Taking extra doses or changing timing without medical guidance can cause medication levels to build to unsafe levels. -
Never mix Seroquel with alcohol or other sedatives unless a doctor has clearly approved it.
Combining substances that slow the nervous system greatly increases the risk of breathing problems and overdose. -
Attend regular follow-up appointments to reassess dose effectiveness and side effects.
Mental health needs can change over time, and a dose that once worked well may later become too strong or unnecessary. -
Use pill organizers or medication reminders to avoid double-dosing.
This is especially important for extended-release tablets, where accidental repeat dosing can be dangerous. -
Store medications securely and out of reach of others.
Safe storage helps prevent accidental ingestion by children, pets, or other household members.
Medication safety is not about restriction—it is about protecting long-term stability, health, and recovery.
When to Seek Long-Term Support?
Emergency treatment can stabilize an overdose, but additional support may be needed to reduce the risk of future harm and address underlying concerns.
-
The overdose occurred intentionally or during a mental health crisis.
This may signal unresolved distress that needs professional attention beyond emergency care. -
Medication misuse is recurring, or doses are being taken outside medical guidance.
Repeated misuse increases the risk of severe complications over time. -
Anxiety about controlling medication use is increasing.
Feeling unable to manage use safely is an important warning sign that support is needed. -
Mental health symptoms remain unstable despite treatment.
Persistent mood changes, agitation, or sleep disruption may indicate that the current plan needs adjustment.
In these situations, coordinated care—including psychiatric follow-up and, when appropriate, substance-use support—can lower overdose risk and help families regain confidence in a safer, more effective treatment plan.
FAQs
An overdose of Seroquel can cause symptoms that range from mild to life-threatening, depending on the dose and individual factors. Common signs include extreme drowsiness, confusion, dizziness, rapid heartbeat, low blood pressure, and difficulty breathing. In more severe cases, a person may experience seizures, loss of consciousness, irregular heart rhythms, or coma. Symptoms can worsen over several hours, making early medical evaluation critical.
Seroquel overdose can be serious and potentially fatal, especially at high doses or when combined with alcohol, opioids, or other sedating medications. The drug can significantly depress the central nervous system and interfere with heart rhythm and blood pressure regulation. Even if symptoms appear mild at first, complications may develop later, which is why all suspected overdoses should be treated as medical emergencies.
If a Seroquel overdose is suspected, seek emergency medical help immediately. Call local emergency services or poison control right away. Do not attempt to induce vomiting or give food or drink unless instructed by a medical professional. If the person is unconscious, having trouble breathing, or experiencing seizures, emergency care is urgent. Prompt treatment can be life-saving and greatly reduces the risk of long-term complications.
Resources
Related Articles
Treatment Centers in Virginia










