What Is Addiction: Causes, Types, Symptoms, Effects, and Treatment

Addiction is a chronic condition marked by compulsive behavior despite harmful consequences. Affecting millions globally, addiction disrupts health, relationships, and productivity, impacting individuals, families, and communities alike. According to the National Institute of Drug Abuse (NIDA), 40.3 million people in the United States had an SUD in 2020, and only 6.5% of people with SUD received treatment.
The main causes of addiction include genetic vulnerability, environmental influences, early exposure to substances, trauma, and co-occurring mental health disorders, all of which alter brain function and increase dependency risk.
Types of addiction include substance addiction and behavioral addiction. Alcohol, opioids, and nicotine are the commonly abused substances. Behavioral addictions, such as gambling or internet use, are driven by a compulsive need for reward or relief through these behaviors.
Common symptoms of addiction include intense cravings, withdrawal, mood changes, secrecy, and neglect of responsibilities. These signs progress gradually, making early detection and intervention critical for recovery.
The effects of addiction extend beyond physical harm to include emotional instability, strained relationships, job loss, legal issues, and long-term cognitive damage, profoundly altering a person's quality of life.
Effective treatment options for addiction range from medical detox and psychotherapy to medication-assisted treatment, dual diagnosis care, and holistic approaches like mindfulness. Long-term recovery depends on ongoing support and individualized care plans.
How Does Addiction Begin and Progress Over Time?
Addiction begins when repetitive exposure to substances or behaviors alters the brain's reward system. Over time, this repeated stimulation leads to changes in brain chemistry, particularly involving dopamine, a key neurotransmitter linked to pleasure and motivation. As the brain becomes conditioned to seek the substance or behavior to maintain a sense of reward, individuals lose control over their actions. According to the National Institute on Drug Abuse (NIDA), over 20 million individuals nationwide suffer from substance use disorders annually.
The progress of addiction over time reinforces compulsive use, despite harmful consequences, as the brain’s natural ability to regulate pleasure and decision-making becomes impaired. Research by the National Institute on Drug Abuse (NIDA) titled “Drugs and the Brain” has shown that addiction fundamentally alters brain chemistry, creating a cycle of dependence. Dopamine levels surge during substance use or addictive behaviors, producing intense feelings of euphoria.
What Sets Addiction Apart from Habits and Physical Dependence?
Addiction is set apart from habits and physical dependence by its compulsive behavior and loss of control. While habits are routine actions and physical dependence involves withdrawal symptoms when stopping a substance, addiction goes further, it compels continued use despite negative consequences, driven by psychological cravings and behavioral compulsion.
In What Ways Does Addiction Impact Brain Function?
Addiction impacts brain function in ways including dysregulation of dopamine pathways, impaired executive function in the prefrontal cortex, and heightened reactivity in the limbic system. Repeated exposure to addictive substances floods the brain with dopamine, particularly in the nucleus accumbens, reinforcing the behavior by creating a powerful reward loop, as studied by Help Guide in “Understanding Addiction: How Addiction Hijacks the Brain.”
Over time, the brain reduces natural dopamine production and receptor availability, a process known as downregulation, leading to tolerance and diminished sensitivity to pleasure. A study by Goldstein RZ, Volkow ND. et al. 2011, titled “Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications,” show that chronic substance use weakens the prefrontal cortex, responsible for impulse control and judgment, while strengthening circuits in the amygdala and hippocampus that drive emotional memory and craving. This neural reorganization underlies compulsive drug-seeking and makes sustained recovery neurologically demanding.
Why Do People Become Addicted?

People become addicted because of a combination of biological, psychological, and social factors that interact to increase vulnerability to substance use and compulsive behaviors. These elements shape how an individual responds to drugs or addictive activities and how likely they are to develop a dependency.
People become addicted for the following reasons:
-
Biological predisposition: Genetics plays a major role in addiction risk. Studies by Learn Genetics Utah suggest that approximately 40% to 60% of a person’s susceptibility to addiction is heritable. Individuals also have differences in brain chemistry, especially in the dopamine reward system, which makes them more sensitive to the pleasurable effects of substances.
-
Psychological factors: Mental health conditions such as anxiety, depression, PTSD, or ADHD co-occur with addiction. People use drugs as a coping mechanism to self-medicate emotional pain, leading to a cycle of dependence that reinforces addictive behavior over time. According to the data, 21.9% to 24.1% of individuals with mood disorders (MD) or anxiety disorders (AD) reported self-medicating (SM) with alcohol and/or drugs, according to a study by Turner S, Mota N, Bolton J, Sareen J. et al. 2018, titled “Self-medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature.”
-
Environmental and social influences: Exposure to high-stress environments, childhood trauma, peer pressure, or drug availability significantly increases the risk of addiction. Adverse life experiences alter stress response systems and brain development, making individuals more vulnerable to the reinforcing effects of substances, as studied by Khoury L, Tang YL, Bradley B, Cubells JF, Ressler KJ. et al. 2010, titled “Substance use, childhood traumatic experience, and Posttraumatic Stress Disorder in an urban civilian population.”
What Factors Contribute to a Higher Risk of Addiction?
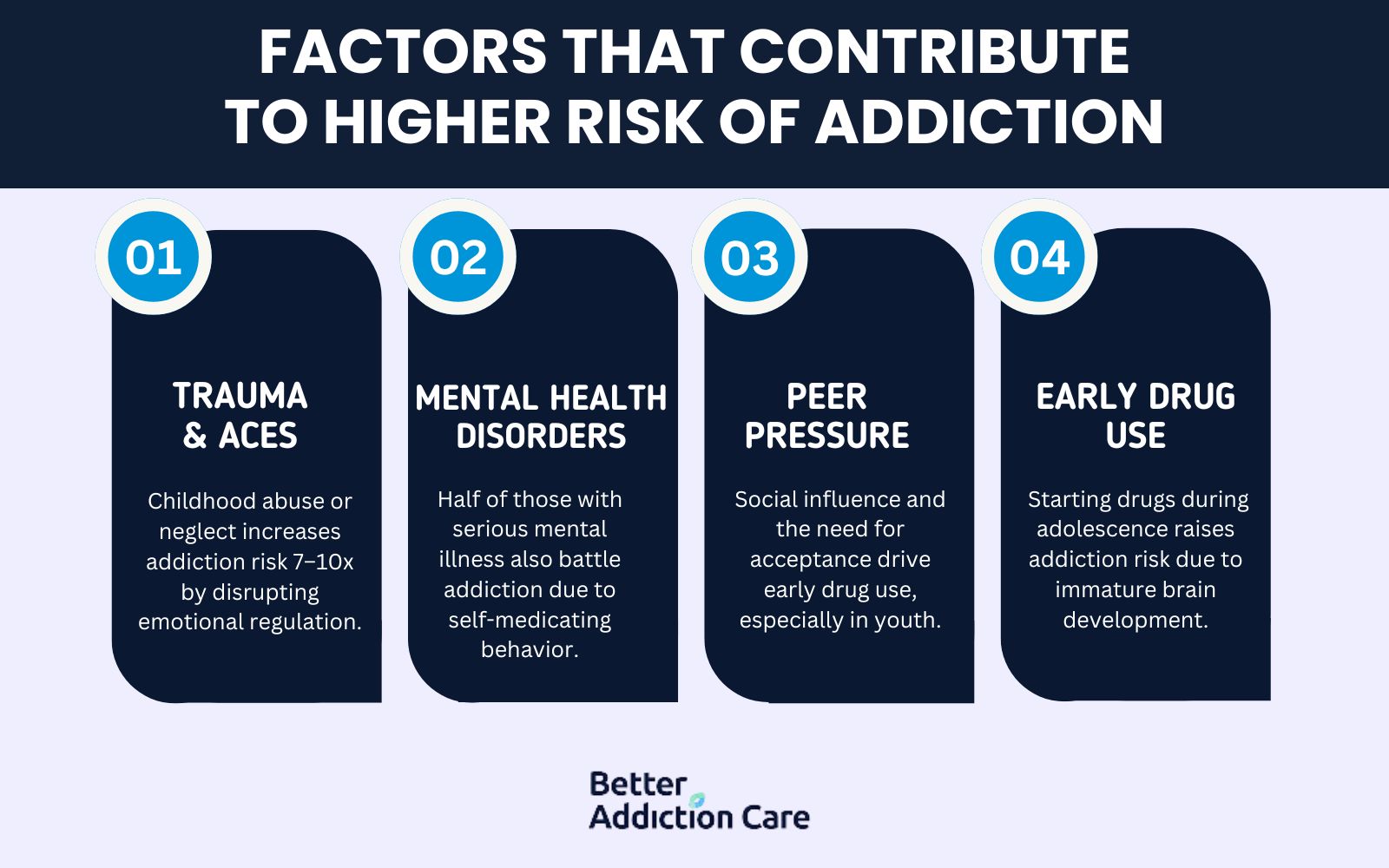
Factors that contribute to the higher risk of addiction include genetic vulnerability, early exposure to trauma, mental health challenges, and environmental influences like peer pressure. These elements interact in complex ways to increase a person's susceptibility to substance use disorders.
The following factors contribute to the higher risk of addiction:
-
Trauma and Adverse Childhood Experiences (ACEs): Exposure to physical, emotional, or sexual abuse, neglect, or witnessing violence during childhood significantly raises the risk of later substance misuse. ACEs disrupt stress regulation and coping mechanisms, making individuals more prone to self-medication. Individuals with an ACE score of 5 or higher are seven to 10 times more likely to use illegal drugs and become addicted, as studied by AFMC.org in “Connecting the Dots: ACEs and Addiction.”
-
Mental Health Disorders: Conditions like depression, anxiety, PTSD, and bipolar disorder co-occur with addiction, as reported by SAMHSA. People turn to drugs or alcohol as a form of self-medication, increasing the likelihood of developing a substance use disorder. Approximately half of individuals with severe mental health disorders also struggle with substance abuse, according to HelpGuide.org. Around 37% of those who abuse alcohol and 53% of drug users have at least one serious co-occurring mental illness.
-
Peer Pressure and Social Influence: Especially among adolescents and young adults, social circles and the desire for acceptance strongly influence experimentation and continued use of addictive substances.
-
Early Drug Use: Initiating substance use during adolescence, when the brain is still developing, particularly the prefrontal cortex, which governs impulse control, significantly increases the risk of long-term addiction, according to a study by Chen CY, Storr CL, Anthony JC. et al. 2009, titled “Early-onset drug use and risk for drug dependence problems.”
Which Groups Are Most Vulnerable to Developing Addiction?
Groups that are most vulnerable to developing addiction include adolescents, individuals with co-occurring mental health disorders, and people with a family history of substance abuse. Teenagers are particularly at risk due to ongoing brain development, especially in areas responsible for impulse control and decision-making, as studied by Winters KC, Arria A. et al., 2011, titled “Adolescent Brain Development and Drugs.”
According to the National Institute on Drug Abuse, early drug use is a strong predictor of later addiction. Individuals with depression, anxiety, or trauma-related disorders also face heightened vulnerability due to the self-medication cycle. Demographic data reveals that males tend to have higher addiction rates than females, while certain ethnic groups experience unique cultural or systemic factors that increase susceptibility.
How Do Co-occurring Mental Health Disorders Complicate Addiction Treatment?
Co-occurring mental health disorders complicate addiction treatment by introducing additional challenges that interfere with recovery. Conditions like anxiety, depression, or PTSD exacerbate addiction symptoms and make it harder for individuals to focus on treatment, leading to a cycle of relapse and emotional distress.
The presence of both a mental health disorder and substance use disorder, known as dual diagnosis, requires an integrated treatment approach that addresses both conditions simultaneously. A study by NIDA in “Common Comorbidities with Substance Use Disorders Research Report” has shown that nearly half of individuals with substance use disorders also have a co-occurring mental health disorder, emphasizing the importance of dual diagnosis programs that combine therapy for both addiction and mental health challenges for more effective outcomes.
What Types of Addiction Are Most Common?
The most common types of addiction are substance addiction and behavioral addiction, both of which significantly impact an individual's life and health. Substance addiction includes dependence on drugs or alcohol, while behavioral addiction involves compulsive behaviors such as gambling or gaming. Each type leads to serious consequences without treatment and support.
The following are the most common types of addiction:
1. Substance Addiction
Substance addiction refers to the compulsive use of substances, leading to physical and psychological dependence. Examples include alcohol, opioids, nicotine, and cocaine. Individuals with substance addiction experience withdrawal symptoms when they try to stop using the substance. The opioid epidemic in the U.S. has led to a sharp increase in opioid-related deaths, with over 70,000 deaths annually attributed to opioid overdoses. This highlights the urgency of addressing substance use disorders.
2. Behavioral Addiction
Behavioral addiction involves compulsive engagement in non-substance-related activities that become detrimental to one's well-being. Common examples include gambling, internet gaming, and shopping. Recent study by Yau YH, Potenza MN. et al. 2015, titled “Gambling disorder and other behavioral addictions: recognition and treatment,” indicate a rising trend in behavioral addictions, with internet gaming disorder and gambling addiction becoming more prevalent, particularly among young people. The American Psychiatric Association now recognizes these behaviors as serious conditions that require professional treatment.
What Are the Common Signs and Symptoms of Addiction?
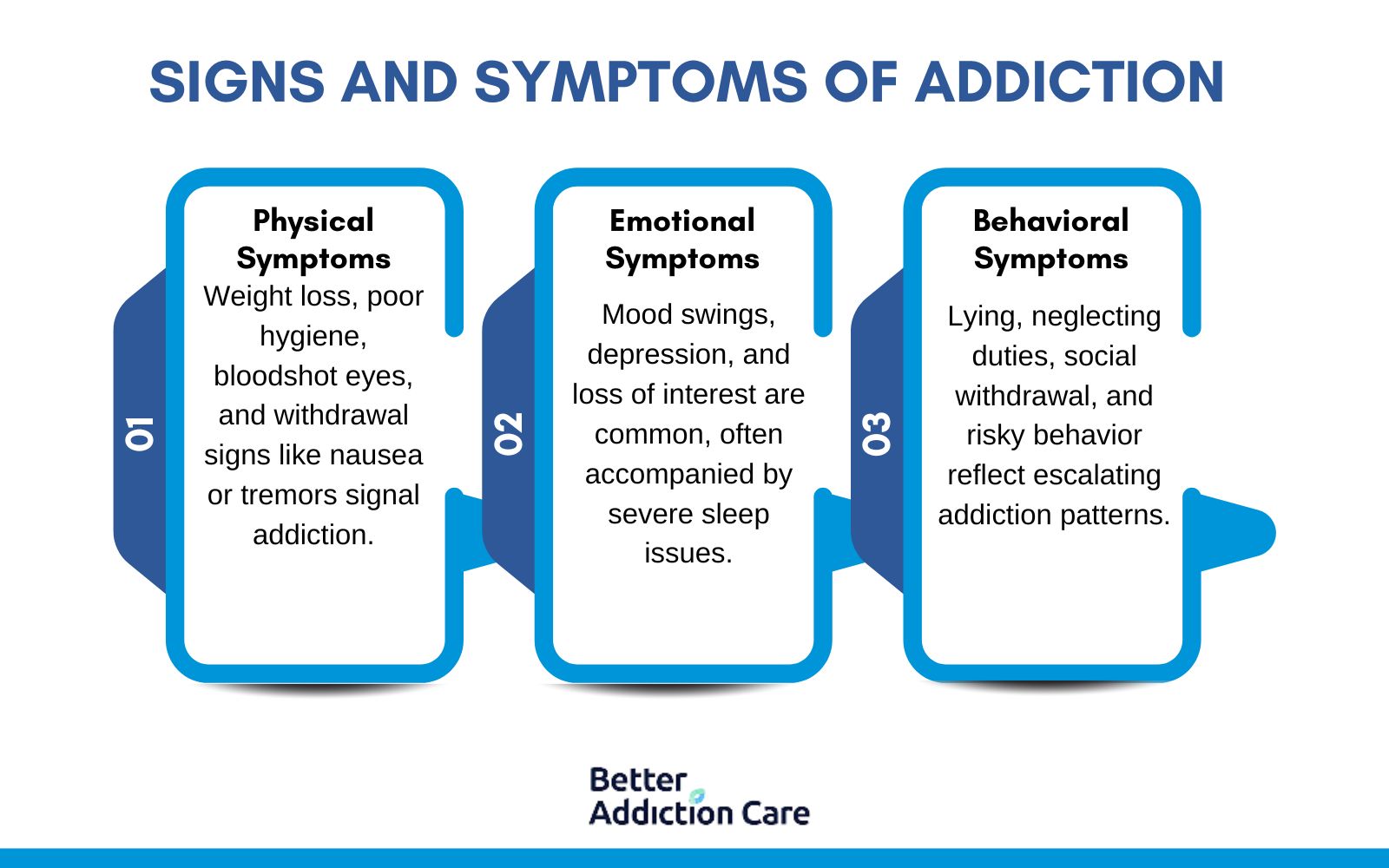
The common signs and symptoms of addiction are categorized into physical, emotional, and behavioral changes that gradually disrupt a person’s daily life. These symptoms vary depending on the type of substance or behavior involved, but they indicate a growing dependence and loss of control.
The following are the common signs and symptoms of addiction:
-
Physical Symptoms: These include changes in appearance such as weight loss, bloodshot eyes, tremors, slurred speech, and poor hygiene. Individuals also experience frequent illnesses or withdrawal symptoms like sweating, nausea, and shakiness when not using the substance. Nearly 80% of individuals with severe addiction experience withdrawal, which ranges from mild discomfort to life-threatening conditions, as studied by Gupta M, Gokarakonda SB, Regina AC, et al., 2024, titled “Withdrawal Syndromes.”
-
Emotional Symptoms: Emotional signs involve mood swings, anxiety, depression, irritability, or a lack of motivation. Over time, the person shows a diminished interest in activities they once enjoyed and develops a sense of hopelessness or emotional numbness. Sleep disturbances are reported by 50 to 70% of individuals with addiction, as studied by Roehrs TA, Roth T., et al., 2015, titled “Sleep Disturbance in Substance Use Disorders.”
-
Behavioral Symptoms: These include secretive behavior, neglecting responsibilities at work or home, financial problems, and frequent lying about usage. Addicted individuals also isolate themselves from friends and family, or associate only with others who support or enable their addiction. Approximately 55% of individuals with addiction report neglecting responsibilities, according to a report by McLean Hospital. Similarly, risk-taking behavior is severe and seen in over 40% of addiction cases, according to a study by Balogh KN, Mayes LC, and Potenza MN. et al. 2013, titled “Risk-taking and decision-making in youth: relationships to addiction vulnerability.”
Which Early Signs of Addiction Often Go Unnoticed?
Early signs of addiction that often go unnoticed are subtle behavioral and emotional changes that are mistaken for stress or personal struggles. Recognizing these indicators early is paramount in preventing the progression of substance use disorders.
Early signs of addiction that often go unnoticed are as follows:
-
Mood Swings and Emotional Instability: Individuals experience sudden or severe mood changes, such as irritability, anger, or unexplained sadness. These fluctuations occur without clear triggers and are linked to the impact of substances on brain chemistry. According to a study by Tolliver BK, Anton RF. et al. 2015, titled “Assessment and treatment of mood disorders in the context of substance abuse,” mood swings are seen in 70% to 80% of individuals with addiction. Similarly, anxiety affects nearly 50% of people with addiction, according to a study by Brady KT, Haynes LF, Hartwell KJ, and Killeen TK. et al. 2013, titled “Substance use disorders and anxiety: a treatment challenge for social workers.”
-
Secretive Behavior: A person might become unusually private, avoiding discussions about their activities or whereabouts. They also lie about minor things or isolate themselves from friends and family, which is a coping mechanism to hide substance use.
-
Financial Difficulties: Unexplained financial problems, such as frequent borrowing of money or missing valuables, are a red flag. These issues arise as individuals prioritize obtaining substances over financial responsibilities.
-
Neglecting Responsibilities: A decline in performance at work or school, missed deadlines, or neglect of household duties indicate that substance use is interfering with daily obligations.
-
Changes in Social Circles Shifting friendships or withdrawing from long-standing relationships occur as individuals seek environments that enable their substance use or as they attempt to conceal their behavior. Social withdrawal occurs in 60-70% of cases, as studied by G.O. Ike K et al., 2020, titled “Social withdrawal: An initially adaptive behavior that becomes maladaptive when expressed excessively.”
-
Physical Appearance and Hygiene: Noticeable changes such as weight fluctuations, poor hygiene, or a general decline in personal care are signs of substance misuse affecting an individual's self-care routines.
-
Sleep Disturbances: Irregular sleep patterns, including insomnia or excessive sleeping, result from the physiological effects of substances or withdrawal symptoms.
What Methods Are Used to Diagnose Addiction?
Methods used to diagnose addiction include clinical interviews, behavioral assessments, and standardized diagnostic tools such as the DSM-5 criteria. Healthcare providers assess patterns of substance use, physical and psychological symptoms, and the impact on daily functioning.
The DSM-5 outlines specific criteria, including tolerance, withdrawal, and continued use despite harm, to help determine the presence and severity of a substance use disorder. Additional tools like the AUDIT (Alcohol Use Disorders Identification Test) or DAST (Drug Abuse Screening Test) are used for more targeted evaluations.
What Are the Effects of Addiction?
The effects of addiction include organ damage, weakened immune function, and increased risk of infectious diseases, especially with injectable substances. Emotionally, individuals suffer from anxiety, depression, and mood instability, as substance use alters brain chemistry and emotional regulation.
Socially, addiction frequently causes strained relationships, job loss, and legal issues. It leads to isolation, as individuals prioritize substance use over social obligations and community ties. Over time, these effects compound, making it more difficult to break the cycle without professional intervention and support systems.
What Treatment Approaches Are Most Effective for Addiction Recovery?

Treatment approaches that are most effective for addiction recovery include medical detoxification, inpatient or outpatient programs, medication-assisted treatment (MAT), psychotherapy, dual diagnosis treatment, experiential therapies, family therapy, and 12-step facilitation. These approaches address the physical, emotional, and psychological dimensions of addiction, offering comprehensive support to promote long-term recovery.
The following treatment approaches are most effective for addiction recovery:
1. Medical Detoxification
Medical detoxification is the initial phase of addiction treatment focused on safely eliminating substances from the body under medical supervision. It ensures physical stabilization and minimizes health risks associated with withdrawal, especially for substances like alcohol, opioids, and benzodiazepines. Withdrawal management during drug detox is important for preparing patients for further therapeutic care. According to Volkow ND et al. 2020, in their study titled “The Science of Drug Use and Addiction,” published by the National Institute on Drug Abuse, medical detox reduces withdrawal complications by up to 80% compared to unsupervised methods like at-home detox.
The following medications are used for addiction detoxification:
-
Benzodiazepines: Benzodiazepine is used for alcohol or sedative withdrawal to prevent seizures and manage anxiety during detoxification under medical supervision.
-
Methadone: Methadone is an opioid agonist that reduces cravings and withdrawal symptoms for individuals detoxing from heroin or prescription opioids.
-
Buprenorphine: Buprenorphine is a partial opioid agonist that eases withdrawal and prevents cravings, commonly used in the early stages of opioid detox.
-
Clonidine: Clonidine helps reduce symptoms like sweating, agitation, and anxiety during opioid withdrawal, though it does not reduce cravings.
2. Inpatient vs. Outpatient Programs
Inpatient and outpatient programs are two core models of addiction treatment that differ in structure, intensity, and setting. Inpatient programs provide a structured environment where individuals live on-site and receive 24/7 care. Outpatient programs offer flexibility, allowing patients to live at home while attending scheduled sessions.
Differences and benefits of each include:
-
Inpatient Treatment: Inpatient rehab offers residential treatment and intensive care, ideal for individuals with severe addiction or co-occurring disorders. According to Keith Humphreys in his publication titled “The Effectiveness of Inpatient Rehabilitation,” published in the Journal of Substance Abuse Treatment (2020), inpatient care increases abstinence success rates by 50% for high-dependency individuals compared to outpatient alternatives.
-
Outpatient Treatment: Outpatient programs provide treatment on a part-time basis, promoting continuity of daily responsibilities and individualized care plans. According to a national report by the Substance Abuse and Mental Health Services Administration titled “Key Substance Use and Mental Health Indicators in the United States,” published by SAMHSA (2022), participants in IOP showed a 55% improvement in long-term alcohol recovery compared to only 30% in unstructured recovery attempts.
Inpatient rehab suits those needing full-time support, whereas outpatient programs are best for those with mild to moderate addiction and a stable home.
3. Medication-Assisted Treatment (MAT)
Medication-Assisted Treatment (MAT) combines FDA-approved medications with counseling and behavioral therapies to treat substance use disorders, especially opioid use disorder and alcohol use disorder. It is an evidence-based approach that significantly improves treatment retention and outcomes.
The following are commonly used medications for different substances:
-
Methadone: Methadone is a long-acting opioid agonist used to reduce cravings and withdrawal symptoms in opioid addiction.
-
Suboxone: Suboxone offers similar benefits as methadone but with a ceiling effect that reduces overdose risk.
-
Naltrexone: Naltrexone is used for both alcohol and opioid addiction; it blocks the euphoric effects of substances.
4. Psychotherapies
Psychotherapies are central to addiction treatment, helping individuals understand and change unhealthy behaviors and thoughts. Approaches like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Motivational Interviewing are widely used to address triggers, coping mechanisms, and relapse prevention.
These therapies support emotional healing and long-term behavioral change and are most effective when tailored to the individual's needs. CBT assists individuals in understanding the triggers and high-risk situations that lead to relapse, as studied by Miller WR, Wilbourne PL. et al. 2002, titled “Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders.”
5. Dual Diagnosis Treatment
Dual diagnosis treatment addresses both addiction and co-occurring mental health disorders such as anxiety, depression, or PTSD. Individuals with co-occurring disorders require integrated care to treat both conditions simultaneously, as untreated mental illness triggers relapse.
Holistic approaches have been shown to increase success rates of addiction treatment, according to a clinical review by Kathleen A. Lynch titled “Complementary and Integrative Approaches to Addiction Treatment,” published in the Journal of Alternative and Complementary Medicine (2019), individuals who incorporated holistic addiction recovery techniques into their treatment experienced a 25% to 30% improvement in anxiety reduction and relapse prevention when used alongside conventional therapies.
6. Experiential Therapies
Experiential therapies use creative and physical activities to support emotional processing and healing. These alternative therapies enhance the mind-body connection, helping individuals express emotions and process trauma outside of traditional talk therapy.
Examples of experiential therapies for addiction treatment include:
-
Art therapy: Art is a creative outlet for exploring emotions. By engaging different areas of the brain, art therapy supports emotional expression, stress relief, and self-esteem. Studies by Shukla A, Choudhari SG, Gaidhane AM, Quazi Syed Z., et al. 2022, titled “Role of Art Therapy in the Promotion of Mental Health: A Critical Review,” show that art and music therapies improve emotional well-being and help individuals cope with recovery-related challenges.
-
Equine Therapy: Equine therapy, also known as equine-assisted therapy, involves structured interactions between individuals in recovery and horses under the guidance of trained professionals. This therapeutic approach helps individuals build confidence, improve emotional regulation, and develop trust and empathy. Horses are highly sensitive to human emotions and behavior, providing immediate, non-judgmental feedback. As clients groom, lead, or care for the animals, they begin to reflect on their own communication patterns, emotional responses, and interpersonal dynamics.
-
Adventure Therapy: Adventure therapy integrates outdoor experiential activities, such as hiking, rock climbing, or ropes courses, into the therapeutic process to build psychological resilience, strengthen coping strategies, and encourage teamwork. This hands-on approach challenges participants to step out of their comfort zones in safe, supportive settings, helping them face fears, manage stress, and build a sense of accomplishment. As individuals engage in physically and emotionally demanding tasks, they develop problem-solving skills, self-confidence, and the ability to work collaboratively.
-
Yoga, Meditation & Mindfulness: In addiction recovery, yoga, meditation, and mindfulness techniques play a valuable role in strengthening the mind-body connection. These practices encourage calmness, self-reflection, and improved emotional control, making them effective tools for managing triggers like stress and cravings. By promoting mental clarity and reducing anxiety, they complement clinical therapies and support long-term healing. Research by Priddy SE, Howard MO, Hanley AW, Riquino MR, Friberg-Felsted K, Garland EL. et al. 2018, titled “Mindfulness Meditation in the Treatment of Substance Use Disorders and Preventing Future Relapse: Neurocognitive Mechanisms and Clinical Implications,” indicates mindfulness-based practices reduce substance use and cravings, supporting long-term sobriety.
-
Acupuncture: Acupuncture is a traditional Chinese therapeutic method that uses fine needle insertion at specific points on the body. It serves as a supportive addiction treatment to help reduce cravings, ease withdrawal symptoms, and regulate stress. Its non-invasive nature and holistic focus make it a useful complement to conventional addiction treatments. Acupuncture is an inexpensive, safe therapy for AUD if administered by trained personnel, as studied by Chen P, Li J, Han X, Grech D, Xiong M, Bekker A, and Ye JH. et al. 2018, titled “Acupuncture for alcohol use disorder.” It effectively reduces alcohol intake, attenuates alcohol withdrawal syndrome, and rebalances the altered release of neurotransmitters and hormones in addiction-related brain areas.
7. Family Therapy
Family therapy involves loved ones in the recovery process to encourage understanding and rebuild trust. This systemic therapy approach improves communication, addresses enabling behaviors, and promotes a healthier home environment. Family involvement is linked to better treatment engagement and long-term recovery success by creating a supportive network around the individual.
8. 12-Step Facilitation
12-Step Facilitation is a structured approach rooted in the principles of programs like Alcoholics Anonymous (AA). It emphasizes accountability, peer support, and spiritual growth, guiding individuals through the steps of admitting powerlessness, making amends, and maintaining sobriety. This 12-step model promotes community, encourages honest self-reflection, and supports long-term commitment to recovery.
Can Addiction Be Fully Cured?
No, addiction cannot be fully cured, but it can be effectively managed. Like other chronic conditions, such as diabetes or hypertension, addiction requires ongoing treatment, support, and behavioral changes. Recovery involves building coping skills, engaging in therapy, and maintaining a strong support system to sustain long-term sobriety and prevent relapse.
Why Do Some People Relapse After Treatment?
Some people relapse after treatment because they face powerful triggers, lack consistent support, or struggle with stress and emotional regulation. Environmental cues, unresolved trauma, or mental health disorders like depression and anxiety also play a role. According to the National Institute on Drug Abuse (NIDA), relapse rates for substance use disorders are similar to those of other chronic diseases, with 40% to 60% of individuals experiencing relapse.
How Can Relapse Be Prevented?
Relapse can be prevented by equipping individuals with effective coping mechanisms, ongoing therapy, and structured support systems. A comprehensive relapse prevention plan focuses on anticipating high-risk situations and developing personalized responses.
The following are the relapse prevention strategies for addiction:
-
Therapy and Counseling: Ongoing participation in cognitive-behavioral therapy (CBT) or other forms of psychotherapy helps individuals identify and manage triggers, replace negative thinking, and reinforce healthy behaviors.
-
Support Groups: Regular attendance at 12-step programs or peer support groups like Narcotics Anonymous (NA) provides accountability and emotional encouragement.
-
Stress Management Techniques: Practicing mindfulness, meditation, or physical exercise helps regulate emotions and reduce the impact of daily stressors that could trigger relapse.
-
Relapse Prevention Plans: Creating a formal strategy that outlines specific steps to take when facing cravings or high-risk situations helps individuals stay on track.
-
Aftercare Programs: Enrolling in outpatient therapy, sober living, or alumni programs ensures continued support and smooth reintegration into daily life post-treatment.
Does Insurance Cover Drug Addiction Treatment?
Yes, most insurance plans do cover drug addiction treatment. Under the Affordable Care Act (ACA), substance use disorder treatment is considered a significant health benefit, meaning insurance providers are required to offer coverage for services like detox, rehab, and therapy. Coverage varies based on the specific plan and provider, so individuals should contact their insurance company to understand what services are included, any copays or deductibles, and which treatment centers are in-network.
How Can Addiction Be Prevented?
Addiction can be prevented through proactive strategies that focus on awareness, early support, and community engagement. Prevention efforts target risk factors before they develop into patterns of substance use or compulsive behaviors.
Addiction can be prevented in the following ways:
-
Education and Awareness: Educating individuals, especially youth, about the risks of substance use and addiction helps build informed decision-making skills. School-based programs, public health campaigns, and family discussions promote early awareness and encourage healthy coping mechanisms.
-
Early Intervention: Identifying and addressing behavioral, emotional, or environmental risk factors early, such as mental health struggles, peer pressure, or trauma, significantly reduces the likelihood of substance use developing into addiction. Support services in schools and communities play a significant role.
-
Community Involvement and Support Systems: Creating strong community networks that offer support, mentorship, and positive social activities helps individuals feel connected and reduces the appeal of risky behaviors. Engaged communities with accessible resources foster resilience and long-term prevention.
What Should You Do If Your Loved Ones Get Addicted?
If your loved ones get addicted, you should respond with compassion, patience, and action. Open, nonjudgmental communication is key, so express concern without blame and let them know you're there to support their recovery journey. Encourage them to seek professional help, such as therapy or treatment programs, and assist in finding appropriate resources. It’s also important to educate yourself about addiction, set healthy boundaries, and, if needed, join support groups like Al-Anon. Being informed and involved creates a stronger support system, which is important for their healing and sustained recovery.
What Is the Prognosis of Addiction?
The prognosis of addiction is highly variable and depends on several factors, including the type and severity of the addiction, co-occurring mental health conditions, and the individual’s support system. While addiction is a chronic condition, long-term recovery is achievable with the right treatment and ongoing care. Consistent engagement in therapy, support networks, and relapse prevention strategies significantly improves outcomes. Many people experience cycles of relapse and recovery, but with continued effort and support, sustained sobriety is possible.
Where to Find Drug Addiction Treatment?
Drug addiction treatment is available through a wide network of specialized rehab centers, outpatient clinics, and mental health providers. Individuals start by contacting their primary care physician or local health department, or using national resources like the treatment center locator. Many treatment centers offer services tailored to specific needs, such as gender-specific programs, dual diagnosis treatment, and holistic care options. Accessible care and early intervention are key to successful recovery.
Related Articles
Treatment Centers in Virginia
 123
123
 123
123
 123
123





