Insurance for Addiction Treatment: Definition, Types, Plans, Costs

Insurance for addiction treatment provides financial support for services related to substance abuse rehabilitation and mental health treatments. According to Strashny, A.’s 2014 study,’ Health insurance status of adult substance abuse treatment admissions aged 26 or older: 2011.’, 59.6% of substance abuse treatment admissions aged 26 or older had no health insurance, while 21.3% had Medicaid, 10.5% had private insurance, and 8.5% had other insurance coverage. Male admissions showed higher rates of uninsurance (63.8%) compared to females (51.2%). Female admissions reported higher Medicaid coverage at 29.7% versus 17.2% for males. Among those referred by the criminal justice system, 67.5% lacked health insurance. This data establishes the pre-Affordable Care Act baseline for health insurance status among substance abuse treatment patients in the United States.
Insurance covers various treatments for substance use disorders, including medical detoxification, residential rehab, partial hospitalization, intensive outpatient care, outpatient therapy, medication-assisted treatment, integrated care for co-occurring disorders, and follow-up counseling.
Insurance for addiction treatment includes both private and public options, with private plans like Aetna, Cigna, Blue Cross Blue Shield, and United Healthcare covering various stages of drug rehab and addiction therapies. Public options include Medicare for seniors, Medicaid for low-income individuals, TRICARE for military families, the Children's Health Insurance Program (CHIP), Veterans Affairs healthcare for veterans, and coverage through the Affordable Care Act, along with specialized programs like Employee Assistance Programs (EAPs) for employer-supported treatment.
Costs associated with addiction treatment insurance include out-of-pocket expenses, differences in coverage between in-network and out-of-network providers, and expenses for detoxification services, rehabilitation programs, and medication therapy. Key costs involve copayments and deductibles, with in-network providers generally offering lower costs, while detox and rehab programs vary significantly in price, though many insurance plans provide some level of coverage for these essential services.
What Is Insurance For Addiction Treatment?
Insurance for addiction treatment is a type of healthcare coverage that financially supports services for substance abuse rehabilitation and addiction-related mental health treatments. This specialized coverage helps pay for various levels of care, including detoxification, inpatient rehabilitation, outpatient programs, and counseling services that address substance use disorders, which are recognized as legitimate medical conditions requiring professional intervention.
The exact benefits vary by plan type, with Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), and Point of Service (POS) plans offering different combinations of provider flexibility, cost structures, and network restrictions. Coverage typically encompasses medical detoxification, residential treatment, Intensive Outpatient Programs (IOP), Partial Hospitalization Programs (PHP), Medication-Assisted Treatment (MAT), behavioral therapy, and aftercare services, though the specific extent of coverage depends on individual policy terms and requires prior authorization.
According to Maclean, J. C.’s 2019 study, ‘The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act, ’ Medicaid-reimbursed prescriptions for medications treating substance use disorders in outpatient settings increased by 43% in expansion states compared to non-expansion states. These increases primarily replaced uninsured patients rather than those with private insurance. Prior to expansion, only 19% of patients in expansion states possessed Medicaid coverage and just 17% utilized Medicaid for treatment payment. The research confirms substantial changes in treatment financing patterns while admission rates remained unchanged between expanding and non-expanding states.
What Are The Types of Addiction Treatment Covered by Insurance?
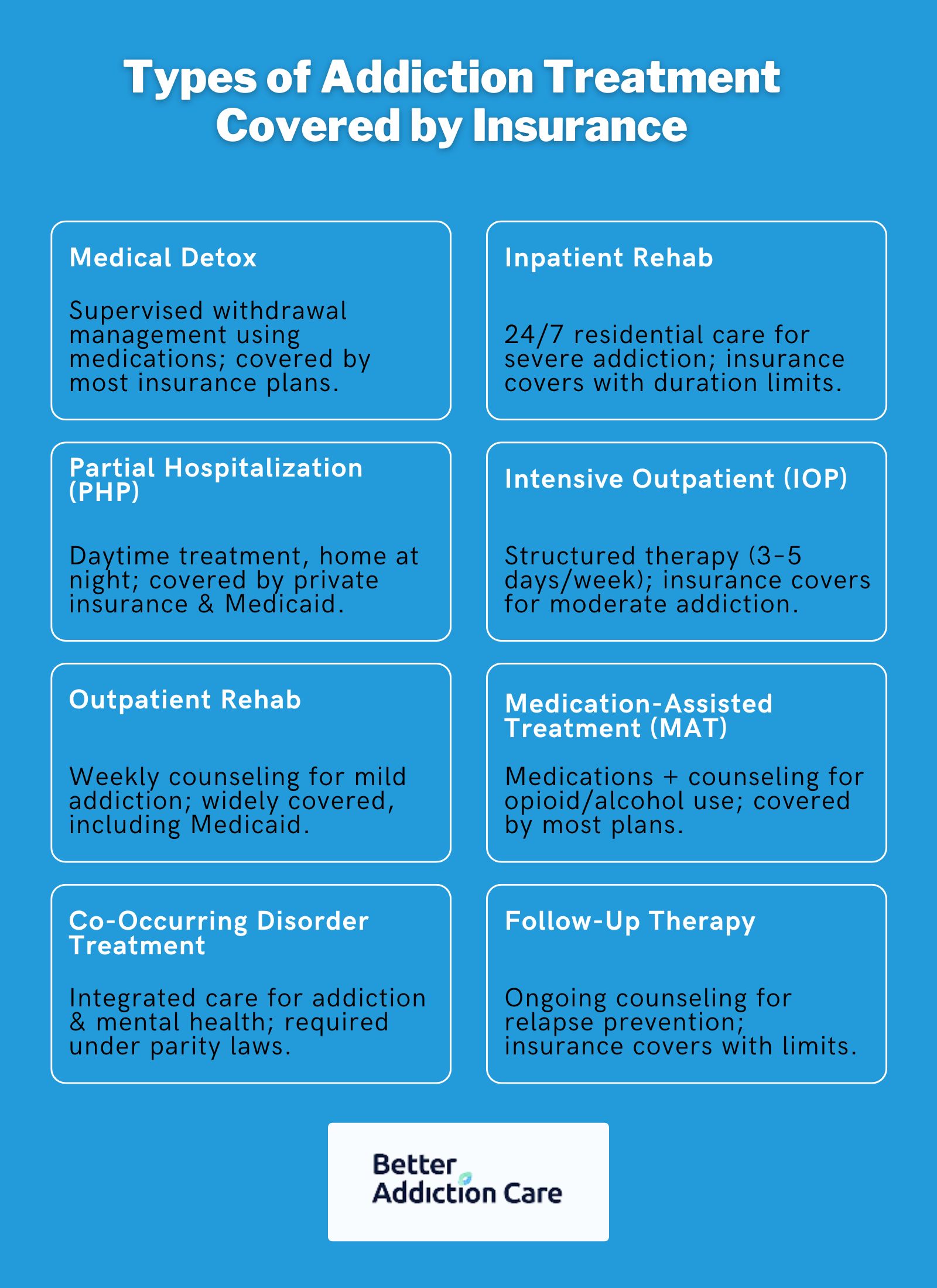
The types of addiction treatment covered by insurance include medically supervised detoxification, residential rehabilitation programs, partial hospitalization options, intensive outpatient care, standard outpatient therapy, medication-assisted treatments, integrated care for co-occurring disorders, and follow-up counseling services.
Here are the key types of addiction treatment options covered by insurance:
-
Medical detoxification: Medical detoxification involves medically supervised withdrawal management using medications to stabilize individuals physically dependent on substances, and most private insurance, Medicaid, and Medicare cover this treatment.
-
Inpatient/residential rehab programs: Inpatient/residential rehab programs are structured, live-in treatment facilities that provide 24/7 medical and therapeutic care for severe addiction cases, and these programs are typically covered by insurance, though duration limits apply.
-
Partial hospitalization programs (PHPs): Partial hospitalization programs (PHPs) involve daytime treatment sessions (5–7 days/week) that allow patients to return home at night, bridging inpatient and outpatient care, and PHPs are often covered by private plans and Medicaid.
-
Intensive outpatient programs (IOPs): Intensive outpatient programs (IOPs) consist of structured therapy sessions (e.g., 3–5 days/week) for moderate addiction, enabling patients to maintain daily responsibilities, and these programs are covered by most insurance plans.
-
Outpatient rehab: Outpatient rehab offers flexible, less-intensive therapy (e.g., weekly counseling) for mild addiction or post-detox maintenance, and this type of treatment is widely covered, including by Medicaid.
-
Medication-assisted treatment (MAT): Medication-assisted treatment (MAT) combines FDA-approved medications (e.g., methadone, buprenorphine) with counseling to treat opioid or alcohol use disorders, and MAT is mandated for coverage under Medicaid and most private plans.
-
Co-occurring disorder treatment: Co-occurring disorder treatment involves integrated care that addresses addiction alongside mental health conditions (e.g., depression, PTSD), and this treatment is required under the Mental Health Parity Act for most plans.
-
Follow-up therapy and counseling: Follow-up therapy and counseling consist of ongoing individual or group sessions aimed at preventing relapse and supporting long-term recovery. These sessions are covered by insurance, though limits exist.
What Insurance Plans Are Available For Addiction Treatment?
Insurance plans available for addiction treatment include both private and public options. Private insurance plans like Aetna, Cigna, Blue Cross Blue Shield, and United Healthcare typically cover various stages of drug rehab and addiction therapies. Public or government-funded insurance options include Medicare for those 65 or older, Medicaid for individuals and families with limited resources, Children's Health Insurance Program (CHIP) for families who don't qualify for Medicaid, Veterans Health Administration (VHA) for veterans, Tricare for military personnel and their families, Indian Health Service (IHS) for American Indians and Alaska Natives, and coverage through the Affordable Care Act (ObamaCare). Additionally, Employee Assistance Programs (EAPs) provide employer-driven systems to assist employees with addiction-related problems.
Here are the common insurance plans available for addiction treatment in detail below:
Private Insurance Plans
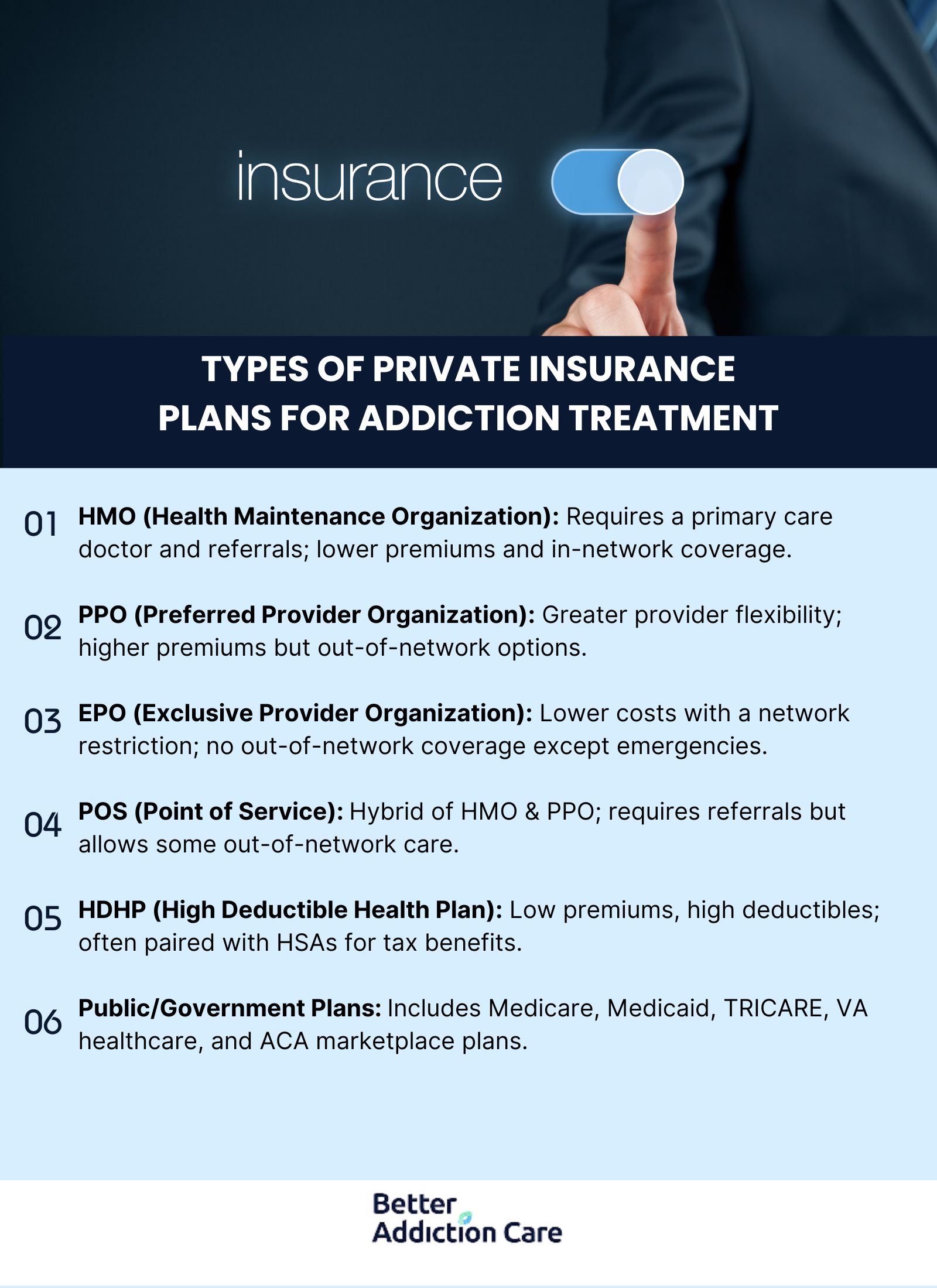
Private Insurance Plans provide coverage options for addiction treatment, including Aetna, Cigna, Blue Cross Blue Shield, and United Healthcare, with various plan structures like Health Maintenance Organization (HMO), Preferred Provider Organization (PPO), Exclusive Provider Organization (EPO), Point of Service (POS), and High Deductible Health Plans (HDHP), each offering different networks, referral requirements, and cost structures for accessing rehab services.
According to Mojtabai, R.’s 2020 study, ‘Private health insurance coverage of drug use disorder treatment: 2005-2018, ’ 37.6% of privately insured Americans with drug use disorders did not know whether their insurance covered addiction treatment. The study examined 11,732 participants between 2005-2018 and found that even among those with confirmed coverage, only 13.4% received treatment in the past year. Drug treatment coverage in private insurance plans increased only modestly from 73.5% in 2005-2013 to 77.5% in 2014-2018 following the Affordable Care Act implementation. The data demonstrates a critical gap between coverage availability and treatment utilization, despite the fact that those with insurance coverage were 2.09 times more likely to receive treatment than those without coverage.
Here are the common types of private insurance plans for addiction treatment:
Health Maintenance Organization (HMO)
HMO plans require patients to select a primary care physician who coordinates all healthcare services, including addiction treatment. These plans typically offer lower premium costs and minimal copayments for in-network services. HMO networks include specific addiction treatment facilities and providers, requiring referrals for specialty addiction services.
Preferred Provider Organization (PPO)
PPO plans provide greater flexibility for addiction treatment, allowing patients to see both in-network and out-of-network providers without referrals. While premiums are typically higher than HMO plans, PPOs offer more treatment facility options and lower out-of-pocket costs when using in-network addiction treatment providers.
Exclusive Provider Organization (EPO)
EPO plans combine elements of both HMO and PPO plans, offering lower premiums while maintaining a network of addiction treatment providers. These plans do not cover out-of-network addiction services except in emergencies, but generally don't require referrals for specialty addiction treatment.
Point of Service (POS)
POS plans resemble HMOs but permit some out-of-network addiction treatment coverage at higher out-of-pocket costs. These plans require referrals from primary care physicians for addiction treatment specialists and facilities, balancing network restrictions with some flexibility.
High Deductible Health Plans (HDHP)
HDHPs feature lower premiums with higher deductibles and are often paired with Health Savings Accounts (HSAs) for addiction treatment expenses. After meeting the deductible, these plans typically cover addiction services at 80-100%, offering tax advantages for treatment costs through the HSA.
Public/Government Insurance Plans
Public/Government insurance plans for addiction treatment include Medicare for seniors and people with disabilities, Medicaid for low-income individuals, TRICARE for military personnel and families, Veterans Affairs healthcare for eligible veterans, Indian Health Service for Native Americans, and coverage through the Affordable Care Act (ObamaCare).
Here are the common Public/Government insurance plans for addiction treatment in detail:
Medicare
Medicare is a federal health insurance program primarily for individuals aged 65 and older, as well as some younger people with disabilities, that offers coverage for addiction treatment through several distinct parts, each addressing different aspects of care.
According to Liu, R.’s 2024 study, ‘Access to treatment before and after Medicare coverage of opioid treatment programs, ’ Medicare coverage of opioid treatment programs (OTPs) since January 2020 produced significant numerical improvements. Medicare acceptance at treatment facilities increased from 21.31% in 2018 to 80.76% in 2021. For-profit OTPs showed greater gains, with acceptance rates rising from 11.67% to 78.46%. Counties with higher non-White populations gained an additional 0.86 Medicare-accepting OTPs on average.
Here are the key parts of Medicare:
-
Medicare Part A: Covers inpatient addiction treatment in hospitals and specialized psychiatric facilities, including room and board, nursing care, and related services.
-
Medicare Part B: Provides coverage for outpatient addiction treatment services, such as individual and group therapy, counseling, patient education, and medication management to support recovery.
-
Medicare Part D: Offers coverage for prescription medications used in addiction treatment, including drugs like Suboxone that are critical for managing substance use disorders.
-
Medicare Advantage (Part C): Combines the benefits of Parts A, B, and often D, and includes additional or enhanced addiction treatment services depending on the specific plan.
Medicaid
Medicaid is a vital federal and state program providing comprehensive addiction treatment services to low-income individuals and families.
According to Olfson, M.’s 2021 study, ‘Medicaid Expansion and Low-Income Adults with Substance Use Disorders.’, Medicaid coverage in expansion states [states that expanded Medicaid in 2014 or earlier] significantly increased from 24.8% in 2012-13 to 48.0% in 2016-17, while uninsured rates dropped from 34.8% to 13.5% during the same period. In non-expansion states [states that did not expand Medicaid], Medicaid coverage grew more modestly from 14.3% to 23.4%. Among those receiving substance use treatment in expansion states, Medicaid coverage rose dramatically from 28.2% to 63.2%. Despite these insurance gains, treatment rates remained low at approximately 12-13%, suggesting that insurance coverage alone does not address all barriers to substance use treatment.
As one of the largest payers for mental health and substance use disorder services in the United States, Medicaid offers critical support through:
-
Core Coverage: Includes essential detoxification services that allow individuals to safely manage withdrawal symptoms under medical supervision before progressing to further treatment.
-
Comprehensive Care: Provides access to evidence-based treatments, including individual and group counseling, behavioral therapy, family therapy, and specialized addiction recovery programs.
-
Medication-Assisted Treatment (MAT): Covers FDA-approved medications for addiction treatment, including opioid agonists and antagonists, along with necessary counseling and behavioral therapies.
-
State-Specific Benefits: While coverage varies by state, all Medicaid programs must cover substance use disorder treatment as an essential health benefit, though the scope and accessibility of services differ.
-
Medicaid Expansion: States that expanded Medicaid under the Affordable Care Act typically offer more robust addiction treatment options, making services accessible to previously ineligible populations.
-
Care Coordination: Many states utilize integrated care models to address both the physical and mental health aspects of addiction, creating more effective treatment pathways for those with substance use disorders.
-
Reduced Financial Barriers: Provides treatment options with minimal out-of-pocket costs, making recovery possible for vulnerable populations who would otherwise be unable to afford care.
TRICARE
TRICARE is a government-sponsored health insurance program providing comprehensive healthcare, including addiction treatment coverage, to military service members, retirees, and their families through various plan options tailored to meet different needs.
According to the Substance Abuse and Mental Health Services Administration (US), & the Office of the Surgeon General (US). 2016, ‘Facing addiction in America: The Surgeon General's report on alcohol, drugs, and health.’, the Department of Defense (DoD) spent approximately $1.2 billion to address problems related to alcohol use in 2006 among TRICARE beneficiaries, including $425 million in medical costs and $745 million in reduced readiness and misconduct.
-
TRICARE Prime: A managed care option offering comprehensive addiction treatment coverage with lower out-of-pocket costs for active-duty members and their families.
-
TRICARE Select: A fee-for-service plan allowing greater flexibility in choosing providers for addiction treatment services.
-
TRICARE Reserve Select: A premium-based plan offering healthcare coverage, including addiction treatment, for eligible National Guard and Reserve members.
-
TRICARE For Life: A Medicare wraparound supplement for military retirees that covers additional addiction treatment costs not fully addressed by Medicare.
Children's Health Insurance Program (CHIP)
The Children's Health Insurance Program (CHIP) is a government program that provides low-cost health coverage to children in families with incomes too high to qualify for Medicaid but too low to afford private insurance. CHIP coverage details vary by state, but it generally includes essential health services for children, such as doctor visits, immunizations, and hospital care, and also covers comprehensive addiction treatment and rehabilitation services when needed. According to the United States Government, CHIP eligibility covers uninsured children under age 19 in families with incomes too high for Medicaid but too low for private insurance. Income thresholds range from 170% to 400% of the Federal Poverty Level, depending on the state. The program serves three populations: children, pregnant women, and targeted low-income children from conception to birth. Applicants must be U.S. citizens or qualified immigrants and residents of their state. States expanded enrollment through strategies like express lane eligibility, continuous eligibility, and presumptive eligibility.
Veterans Affairs (VA) Health Care
Veterans Affairs (VA) Health Care is a federally funded system that provides comprehensive healthcare services to eligible veterans, including a wide range of addiction treatment options such as residential rehabilitation, outpatient care, and access to community providers when needed.
-
Standard VA Health Benefits: Offers comprehensive addiction treatment coverage, including medical services, counseling, and evidence-based therapies like cognitive behavioral therapy.
-
VA Community Care Network: Allows veterans to access addiction treatment from community providers when VA facilities are unable to provide timely care, ensuring continuity of services.
-
VA Residential Rehabilitation Programs: Provides specialized, intensive addiction treatment in inpatient or domiciliary settings, focusing on comprehensive rehabilitation and recovery support.
-
VA Outpatient Addiction Treatment Programs: Delivers regular outpatient services, including individual and group therapies, medication-assisted treatment (MAT), and co-occurring disorder management for substance use disorders.
Indian Health Service (IHS)
The Indian Health Service (IHS) is a federal agency within the Department of Health and Human Services responsible for providing direct healthcare services, including medical, dental, behavioral health, and addiction treatment, to American Indians and Alaska Natives (AI/ANs), with an emphasis on culturally sensitive care. IHS offers a range of substance abuse treatment services, such as outpatient counseling, medication-assisted treatment, detox, residential treatment, and inpatient care, tailored to address both the physical and cultural needs of Native communities.
Affordable Care Act (ObamaCare):
The Affordable Care Act (ACA), also known as ObamaCare, is a comprehensive healthcare reform law enacted in 2010 that mandates all insurance plans, including those offered through the Health Insurance Marketplaces, to provide essential health benefits, including coverage for addiction treatment and rehabilitation services, making these services more accessible and affordable.
According to Olfson, M.’s 2021 study, ‘Effects of the ACA on Health Care Coverage for Adults With Substance Use Disorders, ’ the Affordable Care Act significantly reduced uninsured rates among adults with substance use disorders from 27.8% to 18.7% between 2012-13 and 2015-16. Medicaid coverage for this population increased by 7.3%, while individually purchased private insurance rose by 2.4%. The ACA impact differed between groups, with Medicaid expansion benefiting adults with substance use disorders 2.7% more than those without such disorders. After 2016, coverage gains stalled completely, with uninsured rates remaining virtually unchanged from 2015-16 to 2017-18. These findings demonstrate the ACA's initial effectiveness in expanding coverage but highlight the subsequent stabilization of insurance rates among vulnerable populations.
Employee Assistance Programs (EAPs)
EAPs provide initial assessment, short-term counseling, and referral services for addiction treatment. These employer-sponsored programs typically offer 3-8 free counseling sessions before transitioning to regular insurance coverage.
According to Jacobson, J. M., & Sacco, P.’s 2012 study, ‘Employee assistance program services for alcohol and other drug problems: implications for increased identification and engagement in treatment.’, among adults who sought services for alcohol and other drug (AOD) problems, only 7.58% reported using Employee Assistance Program services for these issues at some point during their lives. The study found that having major depressive disorder, a drug use disorder, and Black race/ethnicity were factors associated with a greater likelihood of seeking EAP services for AOD problems. Research suggests that employees who follow through with their EAP's recommendations demonstrate higher rates of participation and engagement in AOD treatment programs.
Which Are the Most Common Types of Insurance Plans?
The most common types of insurance plans are Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), and Point of Service (POS) plans. HMOs require patients to first see a primary care physician who then provides referrals to specialists when necessary, typically offering lower overall costs.
PPOs offer greater flexibility in choosing healthcare providers, though they come with higher premiums and lower co-pays. POS plans function similarly to HMOs but allow occasional out-of-network care for additional fees. When selecting the right insurance plan, evaluate your provider preferences, budget constraints, and coverage needs. Importantly, inquire specifically about substance abuse treatment coverage in each plan option. Always consult your insurance provider's detailed documentation to make an informed decision that aligns with your specific healthcare requirements.
What Are The Costs Associated With Addiction Treatment Insurance?
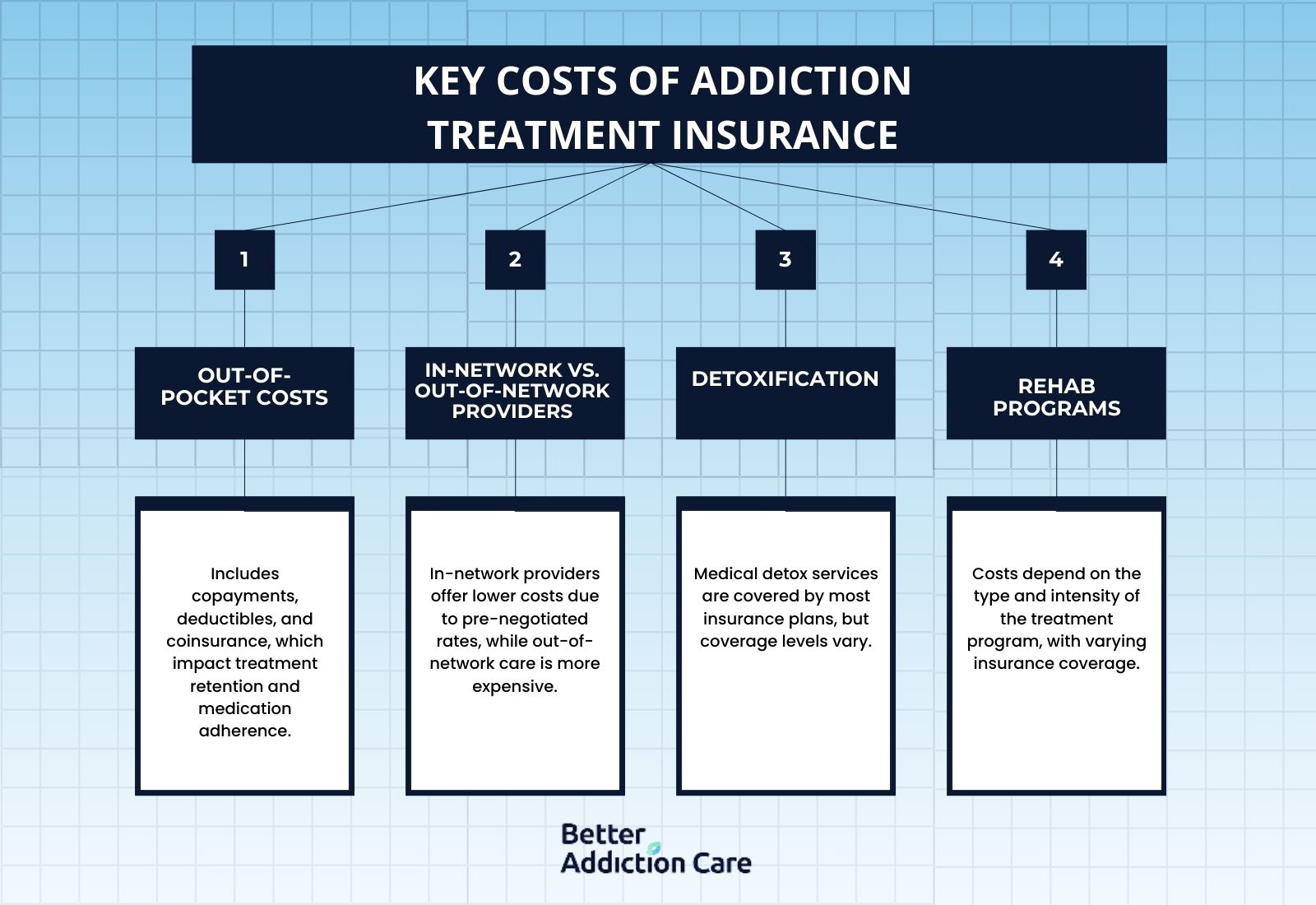
The costs associated with addiction treatment insurance include out-of-pocket expenses, varying coverage between in-network and out-of-network providers, detoxification services, rehabilitation programs, medication therapy, and specialized treatment options.
Here are the key costs associated with addiction treatment insurance:
-
Out-of-Pocket Costs: Even with insurance coverage, individuals still incur out-of-pocket expenses such as copayments, deductibles, or coinsurance. These costs range significantly depending on the insurance plan. According to Dunphy, C.’s 2021 study, ‘Do out-of-pocket costs influence retention and adherence to medications for opioid use disorder?’, higher out-of-pocket costs significantly impact treatment outcomes for patients with opioid use disorder. A $1 increase in daily out-of-pocket buprenorphine cost is associated with a 12-14% decrease in the odds of treatment retention across the 180, 360, and 540-day thresholds. This same $1 increase correlates with a 5-8% increase in the number of days without buprenorphine coverage during each retention period. The researchers observed these effects consistently, demonstrating that cost barriers directly influence both whether patients remain in treatment and their medication adherence when they do continue treatment.
-
In-Network vs. Out-of-Network Providers: In-network providers are healthcare professionals or facilities that have negotiated agreements with insurance plans, resulting in lower out-of-pocket costs for patients. These providers are generally more affordable due to pre-negotiated rates. Out-of-network providers are those that do not have such agreements, and while they are still covered by insurance, they often result in higher costs for the insured individual. Out-of-network care also involves additional charges, such as coinsurance or balance billing, making it less cost-effective compared to in-network options.
-
Detoxification: Medical detox services are often the first step in addiction treatment and are costly. However, most insurance plans provide some level of coverage for detox, though the extent of that coverage varies.
-
Rehab Programs: Rehab programs are structured treatment plans designed to help individuals recover from substance use disorders, and these programs vary in type and intensity to meet the specific needs of patients. According to the National Center for Drug Abuse Statistics, Inpatient rehabilitation programs cost an average of $12,500 for a 30-day program, with longer 60-90 day programs averaging $36,000. Private facility inpatient care averages $575 per day. Outpatient rehabilitation includes standard programs at $5,700 per month or $5,000 for a three-month program, while intensive outpatient care averages $17,250 for 30 days. Partial hospitalization outpatient services average $12,000 for 30 days. The overall average cost of outpatient treatment from the 2016 Census Survey Results stands at $8,386.
Common rehab programs are:
-
-
Inpatient/Residential Rehab: Inpatient or residential rehab programs provide structured, live-in treatment for individuals with severe addiction, and insurance covers a significant portion of these programs, depending on the specifics of the insurance plan.
-
Outpatient Programs: Outpatient programs, including Partial Hospitalization Programs (PHPs) and Intensive Outpatient Programs (IOPs), are generally less expensive than inpatient care. Many insurance plans offer coverage for these services.
-
-
Medication-Assisted Treatment (MAT): MAT involves medications like buprenorphine or methadone, which have associated costs. Most insurance plans, including Medicaid, cover MAT, although copayments or other fees might apply.
-
Specialized Programs: Costs for specialized addiction treatment programs, such as those addressing co-occurring disorders, depend on the provisions of the insurance plan. These programs are often partially or fully covered.
-
Insurance Verification: To determine the exact costs and coverage details, it is essential to verify benefits directly with the insurance provider, as coverage specifics and financial responsibilities vary widely between different plans and insurers.
How Do You Find A Rehab Center That Accepts Your Insurance?
To find a rehab center that accepts your insurance, review your policy documents, contact your provider directly, and confirm coverage specifics before admission to avoid unexpected expenses. Visit Better Addiction Care’s directory of Local drug and alcohol rehab facilities to search for local treatment centers. Call our helpline at (800) 429-7690 for immediate insurance verification. Speak with treatment centers directly about your insurance plan to verify acceptance and understand what services fall under your coverage.
Resources
Related Articles
Treatment Centers in Virginia





